Overview
Ventricular fibrillation is a type of irregular heart rhythm (arrhythmia). During ventricular fibrillation, the lower heart chambers contract in a very rapid and uncoordinated manner. As a result, the heart doesn't pump blood to the rest of the body.
Ventricular fibrillation is an emergency that requires immediate medical attention. It's the most frequent cause of sudden cardiac death.
Emergency treatment for ventricular fibrillation includes cardiopulmonary resuscitation (CPR) and shocks to the heart with a device called an automated external defibrillator (AED). Medications, implanted devices or surgery may be recommended to prevent episodes of ventricular fibrillation.
Ventricular fibrillation may also be called VFib, V-fib or VF.
Symptoms
Collapse and loss of consciousness are the most common symptoms of ventricular fibrillation.
Before a ventricular fibrillation episode, you may have symptoms of an irregularly fast or erratic heartbeat (arrhythmia). You may have:
- Chest pain
- Very fast heartbeat (tachycardia)
- Dizziness
- Nausea
- Shortness of breath
When to see a doctor
Make an appointment with a heart doctor (cardiologist) if you have an unexplained fast or pounding heartbeat.
If you see someone collapse, seek emergency medical help immediately. Follow these steps:
- Call 911 or your local emergency number.
- If the person is unconscious, check for a pulse.
- If no pulse, begin CPR to help keep blood flowing through the body until an automated external defibrillator (AED) is available. The American Heart Association recommends hands-only CPR. Push hard and fast on the person's chest — about 100 to 120 times a minute. It's not necessary to check the person's airway or deliver rescue breaths. Continue until emergency medical help arrives.
- Use an AED as soon as it's available. Deliver a shock following the prompts on the device.
Causes
Ventricular fibrillation is caused by either:
- A problem in the heart's electrical properties
- A disruption of the blood supply to the heart muscle
Sometimes, the cause of ventricular fibrillation is unknown.
To understand more about how ventricular fibrillation occurs, it may be helpful to know how the heart typically beats.
The heartbeat
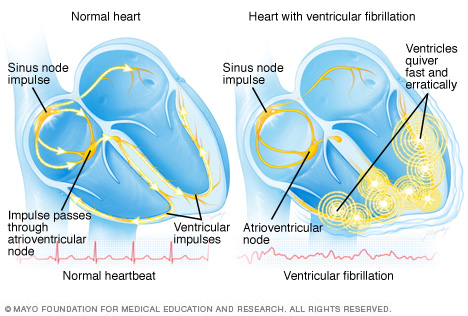
The typical heart has four chambers — two upper chambers (atria) and two lower chambers (ventricles). Within the upper right chamber of the heart (right atrium) is a group of cells called the sinus node. The sinus node is the heart's natural pacemaker. It produces the signals that start each heartbeat.
These electrical signals move across the atria, causing the heart muscles to squeeze (contract) and pump blood into the ventricles.
Next, the signals arrive at a cluster of cells called the AV node, where they slow down. This slight delay allows the ventricles to fill with blood. When the signals reach the ventricles, the lower heart chambers contract and pump blood to the lungs or to the rest of the body.
In a typical heart, this heart signaling process usually goes smoothly, resulting in a typical resting heart rate of 60 to 100 beats a minute. But in ventricular fibrillation, rapid, irregular electrical signals cause the lower heart chambers to quiver uselessly instead of pumping blood.
Risk factors
Things that may increase the risk of ventricular fibrillation include:
- A previous episode of ventricular fibrillation
- A previous heart attack
- A heart problem present at birth (congenital heart defect)
- Heart muscle disease (cardiomyopathy)
- Injuries that cause damage to the heart muscle, such as being struck by lightning
- Drug misuse, especially with cocaine or methamphetamine
- A severe imbalance of potassium or magnesium
Complications
Without immediate treatment, ventricular fibrillation can cause death within minutes. The condition's rapid, erratic heartbeats cause the heart to abruptly stop pumping blood to the body. Blood pressure drops suddenly and significantly. The longer the body lacks blood, the greater the risk of damage to the brain and other organs.
Ventricular fibrillation is the most frequent cause of sudden cardiac death. The risk of other long-term complications depends on how fast treatment is received.
Diagnosis
Ventricular fibrillation is always diagnosed in an emergency situation. If sudden cardiac death has occurred, a pulse check will reveal no pulse.
Tests to diagnose and determine the cause of ventricular fibrillation include:
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which displays the test results. An ECG can show if the heart is beating too fast or too slowly. If you're having an episode of ventricular fibrillation, the ECG usually shows a heartbeat of about 300 to 400 beats a minute.
- Blood tests. Blood tests can be done to check for proteins (enzymes) that leak into the bloodstream when the heart is damaged by a heart attack.
- Chest X-ray. An X-ray image of the chest can show the size and shape of the heart and its blood vessels.
- Echocardiogram. This noninvasive test uses sound waves to create images of the heart in motion. It can show the heart's size and structure.
- Coronary catheterization (angiogram). This test helps health care providers see blockages in the heart arteries. A long, thin flexible tube (catheter) is inserted in a blood vessel, usually in the groin or wrist, and guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video.
- Cardiac computerized tomography (CT). A CT scan uses X-rays to create cross-sectional images of specific parts of your body.
- Cardiac magnetic resonance imaging (MRI). This test uses a magnetic field and computer-generated radio waves to create detailed images of blood flow in the heart.
Treatment
Ventricular fibrillation requires emergency medical treatment to prevent sudden cardiac death. The goal of emergency treatment is to restore blood flow as quickly as possible to prevent organ and brain damage.
Emergency treatment for ventricular fibrillation includes:
- Cardiopulmonary resuscitation (CPR). CPR mimics the pumping motion of the heart. It keeps blood flowing through the body. First call 911 or your local emergency number. Then start CPR by pushing hard and fast on the person's chest — about 100 to 120 compressions a minute. Let the chest rise completely between compressions. Continue CPR until an automated external defibrillator (AED) is available or emergency medical help arrives.
- Defibrillation. This treatment is also called cardioversion. An automated external defibrillator (AED) delivers shocks through the chest wall to the heart. It can help restore a regular heart rhythm. As soon as an AED is available, apply it and follow the prompts. If you're not trained to use an AED, a 911 operator or another emergency medical operator may be able to give you instructions. Public-use AEDs are programmed to recognize ventricular fibrillation and send a shock only when needed.
Other treatments for ventricular fibrillation are given to prevent future episodes and reduce the risk of arrhythmia-related symptoms. Treatment for ventricular fibrillation includes medications, medical devices and surgery.
Medications
Drugs to control the heart rhythm (anti-arrhythmics) are used for emergency or long-term treatment of ventricular fibrillation. If you're at risk of ventricular fibrillation or sudden cardiac death, your provider may prescribe medications to slow and control your heartbeat.
Surgery or other procedures
Surgery or medical procedures to treat ventricular fibrillation include:
- Implantable cardioverter-defibrillator (ICD). An ICD is a battery-powered unit that's implanted under the skin near the collarbone — similar to a pacemaker. The ICD continuously monitors the heart rhythm. If the device detects an episode of ventricular fibrillation, it sends shocks to stop it and reset the heart's rhythm.
- Cardiac ablation. This procedure uses heat or cold energy to create tiny scars in the heart to block the irregular heart signals that cause ventricular fibrillation. It's most often done using thin, flexible tubes called catheters inserted through the veins or arteries. It may also be done during heart surgery.
-
Coronary angioplasty and stent placement. If ventricular fibrillation is caused by a heart attack, this procedure may reduce the risk of future episodes of ventricular fibrillation.
The health care provider inserts a long, thin tube (catheter) through an artery, usually in the groin, to a blocked artery in the heart. A balloon on the tip of the catheter briefly inflates to widen the artery. This restores blood flow to the heart. A metal mesh stent may be placed into the artery to help it stay open.
- Coronary bypass surgery. This open-heart surgery redirects blood around a section of a blocked or partially blocked artery in the heart. It may be done if ventricular fibrillation is caused by coronary artery disease. During bypass surgery, the surgeon takes a healthy blood vessel from the leg, arm or chest. It's connected below and above the blocked artery or arteries in the heart. This creates a new pathway for blood flow.
Lifestyle and home remedies
Lifestyle changes that help keep the heart as healthy as possible include the following:
- Eat a healthy diet. Heart-healthy foods include fruits, vegetables and whole grains, as well as lean protein sources such as soy, beans, nuts, fish, skinless poultry and low-fat dairy products. Avoid added salt (sodium), added sugars and saturated fats.
- Exercise. Physical activity helps you achieve and maintain a healthy weight. Regular exercise helps control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. With your provider's OK, aim for 30 to 60 minutes of physical activity most days of the week. Talk to your health care provider about the amount and type of exercise that's best for you.
- Manage weight. Being overweight increases the risk of heart disease. Talk with your care provider to set realistic goals for body mass index (BMI) and weight.
- Don't smoke. Smoking is a major risk factor for heart disease, especially atherosclerosis. Quitting is the best way to reduce the risk of heart disease and its complications. If you need help quitting, talk to your provider.
- Manage blood pressure and cholesterol. Get regular health checkups to monitor blood pressure and cholesterol. Take medications as prescribed to manage high blood pressure or high cholesterol.
- Limit alcohol. Too much alcohol can damage the heart. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Get regular checkups. Take your medications as prescribed. Have regular follow-up appointments with your health care provider. Tell your provider if your symptoms worsen.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily. Kids often need more. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to your provider about strategies that might help.
Coping and support
Some irregular heart rhythms (arrhythmias) can be triggered by emotional stress. Taking steps to ease stress and anxiety can help keep the heart healthy. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce and manage stress. If you have anxiety or depression, talk to your provider about strategies to help.
Some types of complementary and alternative therapies may help reduce stress, such as:
- Yoga
- Meditation
- Relaxation or mindfulness techniques
Getting support from loved ones may also be helpful.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


