Overview
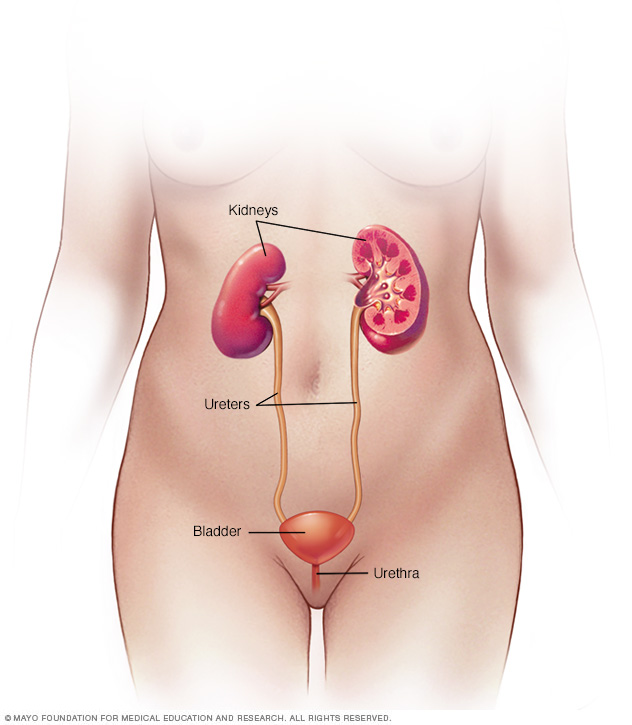
A urinary tract infection (UTI) is an infection in any part of the urinary system. The urinary system includes the kidneys, ureters, bladder and urethra. Most infections involve the lower urinary tract — the bladder and the urethra.
Women are at greater risk of developing a UTI than are men. If an infection is limited to the bladder, it can be painful and annoying. But serious health problems can result if a UTI spreads to the kidneys.
Health care providers often treat urinary tract infections with antibiotics. You can also take steps to lower the chance of getting a UTI in the first place.
Symptoms
UTIs don't always cause symptoms. When they do, they may include:
- A strong urge to urinate that doesn't go away
- A burning feeling when urinating
- Urinating often, and passing small amounts of urine
- Urine that looks cloudy
- Urine that appears red, bright pink or cola-colored — signs of blood in the urine
- Strong-smelling urine
- Pelvic pain, in women — especially in the center of the pelvis and around the area of the pubic bone
In older adults, UTIs may be overlooked or mistaken for other conditions.
Types of urinary tract infections
Each type of UTI may result in more-specific symptoms. The symptoms depend on which part of the urinary tract is affected.
| Part of urinary tract affected | Signs and symptoms |
|---|---|
| Kidneys |
|
| Bladder |
|
| Urethra |
|
When to see a doctor
Contact your health care provider if you have symptoms of a UTI.
Causes
UTIs typically occur when bacteria enter the urinary tract through the urethra and begin to spread in the bladder. The urinary system is designed to keep out bacteria. But the defenses sometimes fail. When that happens, bacteria may take hold and grow into a full-blown infection in the urinary tract.
The most common UTIs occur mainly in women and affect the bladder and urethra.
-
Infection of the bladder. This type of UTI is usually caused by Escherichia coli (E. coli). E. coli is a type of bacteria commonly found in the gastrointestinal (GI) tract. But sometimes other bacteria are the cause.
Having sex also may lead to a bladder infection, but you don't have to be sexually active to develop one. All women are at risk of bladder infections because of their anatomy. In women, the urethra is close to the anus. And the urethral opening is close to the bladder. This makes it easier for bacteria around the anus to enter the urethra and to travel to the bladder.
- Infection of the urethra. This type of UTI can happen when GI bacteria spread from the anus to the urethra. An infection of the urethra can also be caused by sexually transmitted infections. They include herpes, gonorrhea, chlamydia and mycoplasma. This can happen because women's urethras are close to the vagina.
Risk factors
UTIs are common in women. Many women experience more than one UTI during their lifetimes.
Risk factors for UTIs that are specific to women include:
- Female anatomy. Women have a shorter urethra than men do. As a result, there's less distance for bacteria to travel to reach the bladder.
- Sexual activity. Being sexually active tends to lead to more UTIs. Having a new sexual partner also increases risk.
- Certain types of birth control. Using diaphragms for birth control may increase the risk of UTIs. Using spermicidal agents also can increase risk.
- Menopause. After menopause, a decline in circulating estrogen causes changes in the urinary tract. The changes can increase the risk of UTIs.
Other risk factors for UTIs include:
- Urinary tract problems. Babies born with problems with their urinary tracts may have trouble urinating. Urine can back up in the urethra, which can cause UTIs.
- Blockages in the urinary tract. Kidney stones or an enlarged prostate can trap urine in the bladder. As a result, risk of UTIs is higher.
- A suppressed immune system. Diabetes and other diseases can impair the immune system — the body's defense against germs. This can increase the risk of UTIs.
- Catheter use. People who can't urinate on their own often must use a tube, called a catheter, to urinate. Using a catheter increases the risk of UTIs. Catheters may be used by people who are in the hospital. They may also be used by people who have neurological problems that make it difficult to control urination or who are paralyzed.
- A recent urinary procedure. Urinary surgery or an exam of your urinary tract that involves medical instruments can both increase the risk of developing a UTI.
Complications
When treated promptly and properly, lower urinary tract infections rarely lead to complications. But left untreated, UTIs can cause serious health problems.
Complications of a UTI may include:
- Repeated infections, which means you have two or more UTIs within six months or three or more within a year. Women are especially prone to having repeated infections.
- Permanent kidney damage from a kidney infection due to an untreated UTI.
- Delivering a low birth weight or premature infant when a UTI occurs during pregnancy.
- A narrowed urethra in men from having repeated infections of the urethra.
- Sepsis, a potentially life-threatening complication of an infection. This is a risk especially if the infection travels up the urinary tract to the kidneys.
Prevention
These steps may help lower the risk of UTIs:
- Drink plenty of liquids, especially water. Drinking water helps dilute the urine. That leads to urinating more often — allowing bacteria to be flushed from the urinary tract before an infection can begin.
- Try cranberry juice. Studies that look into whether cranberry juice prevents UTIs aren't final. However, drinking cranberry juice is likely not harmful.
- Wipe from front to back. Do this after urinating and after a bowel movement. It helps prevent the spread of bacteria from the anus to the vagina and urethra.
- Empty your bladder soon after having sex. Also drink a full glass of water to help flush bacteria.
- Avoid potentially irritating feminine products. Using them in the genital area can irritate the urethra. These products include deodorant sprays, douches and powders.
- Change your birth control method. Diaphragms, unlubricated condoms or condoms treated with spermicide can contribute to bacterial growth.
Diagnosis
Tests and procedures used to diagnose urinary tract infections include:
- Analyzing a urine sample. Your health care provider may ask for a urine sample. The urine will be looked at in a lab to check for white blood cells, red blood cells or bacteria. You may be told to first wipe your genital area with an antiseptic pad and to collect the urine midstream. The process helps prevent the sample from being contaminated.
- Growing urinary tract bacteria in a lab. Lab analysis of the urine is sometimes followed by a urine culture. This test tells your provider what bacteria are causing the infection. It can let your provider know which medications will be most effective.
- Creating images of the urinary tract. Recurrent UTIs may be caused by a structural problem in the urinary tract. Your health care provider may order an ultrasound, a CT scan or MRI to look for this issue. A contrast dye may be used to highlight structures in your urinary tract.
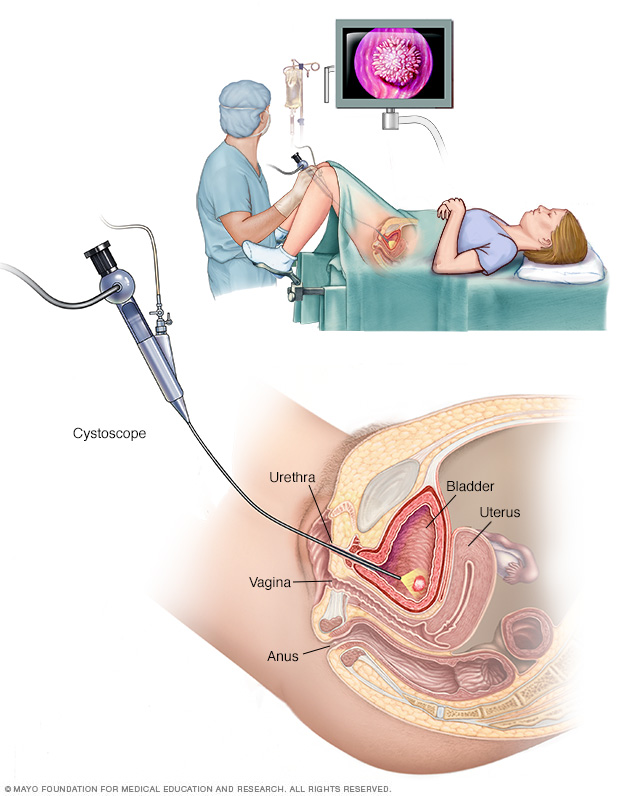
- Using a scope to see inside the bladder. If you have recurrent UTIs, your health care provider may perform a cystoscopy. The test involves using a long, thin tube with a lens, called a cystoscope, to see inside the urethra and bladder. The cystoscope is inserted in the urethra and passed through to the bladder.
Treatment
Antibiotics usually are the first treatment for urinary tract infections. Your health and the type of bacteria found in your urine determine which medicine is used and how long you need to take it.
Simple infection
Medicines commonly used for simple UTIs include:
- Trimethoprim and sulfamethoxazole (Bactrim, Bactrim DS)
- Fosfomycin (Monurol)
- Nitrofurantoin (Macrodantin, Macrobid, Furadantin)
- Cephalexin
- Ceftriaxone
The group of antibiotics known as fluoroquinolones isn't commonly recommended for simple UTIs. These drugs include ciprofloxacin (Cipro), levofloxacin and others. The risks of these drugs generally outweigh the benefits for treating uncomplicated UTIs.
In cases of a complicated UTI or kidney infection, your health care provider might prescribe a fluoroquinolone medicine if there are no other treatment options.
Often, UTI symptoms clear up within a few days of starting treatment. But you may need to continue antibiotics for a week or more. Take all of the medicine as prescribed.
For an uncomplicated UTI that occurs when you're otherwise healthy, your health care provider may recommend a shorter course of treatment. That may mean taking an antibiotic for 1 to 3 days. Whether a short course of treatment is enough to treat your infection depends on your symptoms and medical history.
Your health care provider also may give you a pain reliever to take that can ease burning while urinating. But pain usually goes away soon after starting an antibiotic.
Frequent infections
If you have frequent UTIs, your health care provider may recommend:
- Low-dose antibiotics. You might take them for six months or longer.
- Diagnosing and treating yourself when symptoms occur. You'll also be asked to stay in touch with your provider.
- Taking a single dose of antibiotic after sex if UTIs are related to sexual activity.
- Vaginal estrogen therapy if you've reached menopause.
Severe infection
For a severe UTI, you may need IV antibiotics in a hospital.
Lifestyle and home remedies
Urinary tract infections can be painful, but you can take steps to ease discomfort until antibiotics treat the infection. Follow these tips:
- Drink plenty of water. Water helps to dilute your urine and flush out bacteria.
- Avoid drinks that may irritate your bladder. Avoid coffee, alcohol, and soft drinks containing citrus juices or caffeine until the infection has cleared. They can irritate your bladder and tend to increase the need to urinate.
- Use a heating pad. Apply a warm, but not hot, heating pad to your belly to help with bladder pressure or discomfort.
Alternative medicine
Many people drink cranberry juice to prevent UTIs. There's some indication that cranberry products, in either juice or tablet form, may have properties that fight an infection. Researchers continue to study the ability of cranberry juice to prevent UTIs, but results aren't final.
There's little harm in drinking cranberry juice if you feel it helps you prevent UTIs, but watch the calories. For most people, drinking cranberry juice is safe. However, some people report an upset stomach or diarrhea.
But don't drink cranberry juice if you're taking blood-thinning medication, such as warfarin (Jantovin).
Preparing for an appointment
Your primary care provider, nurse practitioner or other health care provider can treat most UTIs. If you have frequent UTIs or a chronic kidney infection, you may be referred to a health care provider who specializes in urinary disorders. This type of doctor is called a urologist. Or you may see a health care provider who specializes in kidney disorders. This type of doctor is called a nephrologist.
What you can do
To get ready for your appointment:
- Ask if there's anything you need to do in advance, such as collect a urine sample.
- Take note of your symptoms, even if you're not sure they're related to a UTI.
- Make a list of all the medicines, vitamins or other supplements that you take.
- Write down questions to ask your health care provider.
For a UTI, basic questions to ask your provider include:
- What's the most likely cause of my symptoms?
- Are there any other possible causes?
- Do I need any tests to confirm the diagnosis?
- What factors do you think may have contributed to my UTI?
- What treatment approach do you recommend?
- If the first treatment doesn't work, what will you recommend next?
- Am I at risk of complications from this condition?
- What is the risk that this problem will come back?
- What steps can I take to lower the risk of the infection coming back?
- Should I see a specialist?
Don't hesitate to ask other questions as they occur to you during your appointment.
What to expect from your doctor
Your health care provider will likely ask you several questions, including:
- When did you first notice your symptoms?
- Have you ever been treated for a bladder or kidney infection?
- How severe is your discomfort?
- How often do you urinate?
- Are your symptoms relieved by urinating?
- Do you have low back pain?
- Have you had a fever?
- Have you noticed vaginal discharge or blood in your urine?
- Are you sexually active?
- Do you use contraception? What kind?
- Could you be pregnant?
- Are you being treated for any other medical conditions?
- Have you ever used a catheter?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


