Overview
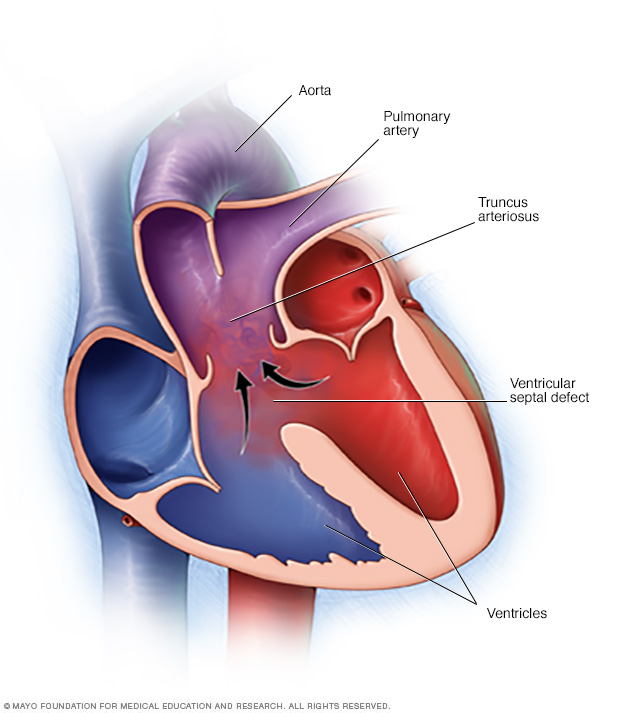
Truncus arteriosus (TRUNG-kus ahr-teer-e-O-sus) is a rare heart condition present at birth. That means it's a congenital heart defect. In this condition, one large blood vessel leads out of the heart, instead of two.
Having only one large blood vessel means that oxygen-poor and oxygen-rich blood mix. This mixing reduces the amount of oxygen delivered to the body. It usually increases the amount of blood flow into the lungs too. The heart has to work harder to adjust for the changes in blood flow.
A baby, also called a fetus, with truncus arteriosus also usually has a hole between the two lower heart chambers, called the ventricles. The hole is called a ventricular septal defect.
Another name for truncus arteriosus is common arterial trunk.
Symptoms
Symptoms of truncus arteriosus most often occur in the first few days of life. They include:
- Blue or gray skin due to low oxygen levels.
- Extreme sleepiness.
- Poor feeding.
- Poor growth.
- Pounding heartbeat.
- Fast breathing.
- Shortness of breath.
When to see a doctor
If you are worried about your baby's feedings, sleep patterns or growth, contact a healthcare professional for an appointment.
Always seek emergency medical care if a baby has any of the following:
- Blue or gray skin.
- Fast breathing.
- Shallow breathing.
- Any breathing trouble.
Causes
Truncus arteriosus occurs as a baby's heart forms during pregnancy. There's often no clear cause. Genetics and environmental factors may play a role.
How the heart works
To understand more about truncus arteriosus, it may be helpful to know how the heart typically works.
The typical heart has four chambers. They are:
- The right upper chamber, also called the right atrium. This heart chamber receives oxygen-poor blood from the body.
- The right lower chamber, also called the right ventricle. This heart chamber pumps blood into the lungs through a large vessel called the pulmonary artery. The blood flows through the pulmonary artery into smaller vessels in the lungs where blood picks up oxygen.
- The left upper chamber, also called the left atrium. This heart chamber receives oxygen-rich blood from the lungs through vessels called pulmonary veins.
- The left lower chamber, also called the left ventricle. This chamber pumps the oxygen-rich blood to the body through the body's largest blood vessel, called the aorta.
A baby's heart before birth
The way the unborn baby's heart forms during pregnancy is complex. At some point, there is a single large blood vessel leading out of the heart. The vessel is called the truncus arteriosus. It usually splits in two as the unborn baby grows in the womb. One part becomes the lower end of the body's main artery, called the aorta. The other part becomes the lower part of the pulmonary artery.
But in some babies, the truncus arteriosus never splits. The wall separating the two lower heart chambers hasn't closed all the way. This results in a large hole between those chambers, called a ventricular septal defect.
Babies with truncus arteriosus also often have a problem with the heart valve that controls blood flow from the lower heart chambers to the single vessel. This valve may not close all the way when the heart relaxes. Blood can move the wrong way, back into the heart. This is called truncal valve regurgitation.
Risk factors
The exact cause of truncus arteriosus is unknown. But some things might increase the risk of a heart problem at birth. Risk factors include:
- Viral illness during pregnancy. Some infections can hurt a developing baby. For example, having German measles during pregnancy can cause changes in a baby's heart development. German measles also is called rubella.
- Poorly controlled diabetes during pregnancy. Careful control of your blood sugar before and during pregnancy can reduce the risk of heart problems in your baby. If you have diabetes, work with your healthcare professional to be sure blood sugar is well controlled before getting pregnant.
- Some medicines taken during pregnancy. Some medicines can cause heart problems and other health conditions in a baby. Tell your healthcare professional about all the medicines you take, including those bought without a prescription.
- Some chromosomal disorders. An extra or irregular chromosome increases the risk of truncus arteriosus. Examples are DiGeorge syndrome, also called 22q11.2 deletion syndrome, and velocardiofacial syndrome.
- Smoking during pregnancy. If you smoke, quit. Smoking during pregnancy increases the risk of heart conditions in your baby.
- Alcohol use. Drinking alcohol during pregnancy increases the risk of heart conditions and other health issues in a baby.
- Obesity. Obesity increases the risk of giving birth to a baby with a heart
Complications
Truncus arteriosus causes severe problems with how blood flows through the lungs, heart and rest of the body.
Complications of truncus arteriosus in babies include:
- Breathing problems. Extra fluid and blood in the lungs can make it difficult to breathe.
- High blood pressure in the lungs, also called pulmonary hypertension. This condition causes the blood vessels in the lungs to narrow. It becomes hard for the heart to pump blood into the lungs.
- Enlargement of the heart. Pulmonary hypertension and increased blood flow strain the heart. The heart must work harder to pump blood. This causes the heart muscle to grow larger. The enlarged heart gradually weakens.
- Heart failure. In this condition, the heart cannot supply the body with enough blood. Too little oxygen and too much strain on the heart can lead to heart failure.
Infants who had their hearts successfully fixed with surgery may still have complications later in life. Possible complications are:
- Pulmonary hypertension that gets worse.
- Backward flow of blood through a heart valve, called regurgitation.
- Irregular heartbeats, called arrhythmias.
Common symptoms of these complications include:
- Dizziness.
- Feeling very fast, fluttering heartbeats.
- Feeling very tired.
- Shortness of breath when exercising.
- Swelling of the belly, legs or feet.
Truncus arteriosus in adults
In rare cases, some people born with truncus arteriosus can survive without heart surgery. They may live into adulthood. But those with the condition will almost certainly have heart failure and develop a complication called Eisenmenger syndrome. This syndrome is caused by permanent lung vessel damage. It results in a significant lack of blood flow to the lungs.
Prevention
Because the cause is unclear, it may not be possible to prevent truncus arteriosus. Getting good prenatal care is important. If you or someone in your family had a heart condition present at birth, talk to your healthcare professional before getting pregnant. You might need to see a genetic counselor and a heart doctor, called a cardiologist.
If you decide to get pregnant, taking these steps can help keep your baby healthy:
- Get recommended vaccinations. Some infections can be harmful to a developing baby. For example, having German measles — also called rubella —during pregnancy can cause changes in a baby's heart development. A blood test done before pregnancy can show if you're immune to rubella. A vaccine is available for those who aren't immune.
- Talk to your healthcare professional about your medicines. Check with your healthcare professional before taking any medicines if you're pregnant or thinking about getting pregnant. Many drugs aren't recommended for use during pregnancy because they can harm a developing baby.
- Take a folic acid supplement. Take a multivitamin with folic acid. Taking 400 micrograms of folic acid daily has been shown to reduce brain and spinal cord conditions in babies. It may help reduce the risk of heart conditions present at birth too.
- Control diabetes. If you have diabetes, ask your healthcare professional how to best manage the disease during pregnancy.
Diagnosis
Truncus arteriosus is usually diagnosed soon after a child is born. The baby may look blue or gray and have trouble breathing.
When a baby is born, a healthcare professional always listens to the baby's lungs to check breathing. If a baby has truncus arteriosus, the healthcare professional may hear fluid in the lungs during this exam. The healthcare professional also listens to the baby's heart to check for irregular heartbeats or a whooshing sound, called a murmur.
Tests
Tests to diagnose truncus arteriosus include:
- Pulse oximetry. A sensor placed on the fingertip records the amount of oxygen in the blood. Too little oxygen may be a sign of a heart or lung problem.
- Chest X-ray. This test shows the condition of the heart and lungs. It can show the size of the heart. A chest X-ray also can tell if the lungs have extra fluid.
- Echocardiogram. An echocardiogram uses sound waves to create pictures of the beating heart. This is the main test to diagnose truncus arteriosus. It shows blood flow through the heart and heart valves. In a baby with truncus arteriosus, the test shows one single large vessel leading from the heart. There's typically a hole in the wall between the lower heart chambers.
Treatment
Infants with truncus arteriosus need surgery to improve blood flow and oxygen levels. Many procedures or surgeries might be needed, especially as a child grows. Medicines might be given before surgery to help improve heart health.
Children and adults with surgically repaired truncus arteriosus need regular health checkups for life.
Medications
Some of the medicines that might be given before truncus arteriosus surgery include:
- Water pills. Also called diuretics, these medicines help the kidneys remove extra fluid from the body. Fluid buildup is a common symptom of heart failure.
- Positive inotropes. These medicines help the heart pump stronger, which improves blood flow. They also help control blood pressure. Positive inotropes may be given by IV to treat severe heart failure symptoms.
Surgery or other procedures
Most infants with truncus arteriosus have surgery within the first few weeks after birth. The specific type of surgery depends on the baby's condition. Usually, the baby's surgeon:
- Rebuilds the single large vessel and aorta to create a new, complete aorta.
- Separates the upper part of the pulmonary artery from the single large vessel.
- Uses a patch to close the hole between the two lower heart chambers.
- Places a tube and valve to connect the right lower heart chamber with the upper pulmonary artery. This creates a new, complete pulmonary artery.
The tube used to create the new pulmonary artery doesn't grow with a child. Follow-up surgeries are needed to replace the tube as the child grows.
Future surgeries may be done with a flexible tube called a catheter. This avoids the need for open-heart surgery. The healthcare professional inserts the catheter into a blood vessel in the groin and guides it to the heart. A new valve can be delivered through the catheter to the proper area.
Sometimes a small balloon at the tip of the catheter is inflated at the site of a blockage, making a blocked artery wider. This procedure is called balloon angioplasty.
After surgery for truncus arteriosus, a person needs lifelong follow-up care with a heart doctor specializing in congenital disease. This type of healthcare professional is called a congenital cardiologist.
Lifestyle and home remedies
If you or your child had truncus arteriosus, your healthcare professional may recommend taking a few steps to protect the heart.
- Exercise limits. Some people with heart conditions need to limit exercise and sports activities, especially competitive sports. Ask your healthcare professional which sports and types of exercise are safe for you or your child. People with Eisenmenger syndrome should avoid strenuous physical activity.
- Antibiotics. Sometimes, heart conditions can increase the risk of infection in the lining of the heart or heart valves. This infection is called infective endocarditis. Antibiotics may be recommended to prevent infections before dental procedures and other surgeries. It's also important to have good oral hygiene and regular dental checkups
-
Pregnancy. If you've had truncus arteriosus repair surgery and want to become pregnant, talk to your healthcare professional first. Ask about the possible risks and complications. It's best to be checked by healthcare professionals with training in adult congenital heart disease and high-risk pregnancies. Together, you and your care team can discuss and plan for any special care needed during pregnancy.
Depending on the level of lung damage that occurred before truncus arteriosus surgery, pregnancy might or might not be recommended. Pregnancy is considered very high risk for those with Eisenmenger syndrome and is not recommended.
Coping and support
Caring for a baby with a serious heart problem, such as truncus arteriosus, can be challenging. Here are some strategies that might be helpful.
- Seek support. Ask for help from family members and friends. Connecting with others in support groups may help manage stress. Contact nonprofit organizations, such as the American Heart Association.
-
Keep track of your baby's health history. Include details about any diagnosis, medicines, surgeries and other procedures. Note the dates for surgeries and procedures. Include dosages for medicines. Write down any healthcare professionals' names and phone numbers.
If possible, get a copy of medical reports. This information helps you remember who provided care. It's also helpful to healthcare professionals who are unfamiliar with your child's health history.
- Talk about your concerns. You might worry about the risks of strenuous activity, especially after heart repair surgery. Ask your child's heart doctor, called a pediatric cardiologist, which activities are safe for your child.
Preparing for an appointment
What you can do
If possible, ask your family members about their medical history. Heart problems at birth can be passed down through families. So it's helpful to know if anyone in your child's family has a history of early heart problems.
Also make a list of questions to ask your baby's healthcare professional. Preparing this list can help you and your healthcare team make the most of your time together. Here are some questions you might want to ask:
- What tests are needed?
- What are the treatment options?
- What are the possible side effects or complications of treatment?
- How do we check for complications?
- What is the long-term outlook for my child?
- My baby has other health conditions. How do we best manage them together?
- If I have another baby in the future, what are the chances of this happening again?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your child's healthcare professional typically asks the following questions:
- Does your baby ever look blue or gray?
- How long are feeding times?
- How much does your baby drink?
- How often and how long does your baby sleep?
- How does your baby respond to touch?
- Does your baby ever breathe fast?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


