Overview
A tonic-clonic seizure, previously known as a grand mal seizure, causes a loss of consciousness and violent muscle contractions. It's the type of seizure most people picture when they think about seizures.
During a seizure, there's a burst of electrical activity in the brain that causes changes in behavior and movements. Seizures can be focal, meaning the burst of electrical activity happens in one area of the brain. Or seizures can be generalized, in which they result in electrical activity in all areas of the brain. Tonic-clonic seizures may begin as focal seizures in a small area of the brain and spread to become generalized seizures that involve the whole brain.
Focal and generalized seizures have different symptoms. People who have generalized seizures usually lose consciousness. But people who have focal seizures may or may not lose consciousness. In tonic-clonic seizures, the muscles become stiff, causing the person to fall. Then the muscles alternately flex and relax.
Usually, a tonic-clonic seizure is caused by epilepsy. But sometimes this type of seizure can be triggered by other health problems, such as a high fever or damage to the brain.
Some people who have a tonic-clonic seizure don’t have another one and don't need treatment. But someone who has recurrent seizures may need treatment with daily anti-seizure medicines to control and prevent future tonic-clonic seizures. Surgery and dietary changes also may be options to manage your seizures.
Symptoms
Tonic-clonic seizures have two stages:
- Tonic phase. Often, someone in the tonic phase will make a sound, such as a groan or yell. The muscles suddenly get stiff and cause the person to fall down. Loss of consciousness occurs. This phase tends to last about 10 to 20 seconds.
- Clonic phase. The muscles go into rhythmic contractions. The arms and legs often jerk. They alternately flex and relax. Convulsions usually last 1 to 2 minutes or less.
The following symptoms occur in some but not all people with tonic-clonic seizures:
- Loss of bowel and bladder function. This may happen during or following a seizure.
- Not responding after convulsions. The person may not become conscious for several minutes after convulsions have ended.
- Confusion. The person often is disoriented after a tonic-clonic seizure. This is referred to as postictal confusion.
- Fatigue. Sleepiness is common after a tonic-clonic seizure.
- Bad headache. Headaches may occur after a tonic-clonic seizure.
When to see a doctor
Call 911 or emergency medical help if:
- The seizure lasts more than five minutes.
- Breathing or consciousness doesn't return after the seizure stops.
- A second seizure follows immediately.
- You have a high fever.
- You're experiencing heat exhaustion.
- You're pregnant.
- You have diabetes.
- You've injured yourself during the seizure.
If you experience a seizure for the first time, see a healthcare professional.
Also see a healthcare professional if you or your child:
- Experiences an increasing number of seizures for no apparent reason.
- Notices new seizure symptoms.
Causes
The brain's nerve cells typically communicate by sending electrical and chemical signals across the synapses that connect the cells. A synapse is the area between cells that allows them to send messages. Tonic-clonic seizures occur when there's a surge of electrical activity over the surface of the brain. Many nerve cells fire at once, much faster than usual. Exactly what causes these changes often is not known.
However, tonic-clonic seizures are sometimes caused by other health problems, such as:
- Injury or infection. Severe head injuries can cause tonic-clonic seizures. Other possible causes include infections, such as encephalitis or meningitis, or having these infections in the past. Stroke and dementias that cause degeneration in the brain, such as Alzheimer's disease, also can cause tonic-clonic seizures.
- Congenital or developmental factors. These can include blood vessels that don't form properly in the brain and brain tumors.
- Metabolic issues. Very low blood levels of glucose, sodium, calcium or magnesium can cause tonic-clonic seizures.
- Withdrawal syndromes. These can include using or withdrawing from drugs, including alcohol.
Risk factors
Risk factors for tonic-clonic seizures include:
- A family history of seizure disorders.
- Any injury to the brain from trauma, a stroke, previous infection and other causes.
- Sleep deprivation.
- Medical problems that affect the balance of minerals in the body.
- Illicit drug use.
- Heavy alcohol use.
Complications
Having a seizure at certain times can be dangerous for you or others. You might be at risk of:
- Falling. If you fall during a seizure, you can injure your head or break a bone.
- Drowning. If you have a seizure while swimming or bathing, you're at risk of accidental drowning.
- Car accidents. A seizure that causes either loss of awareness or control can be dangerous if you're driving a car or operating other equipment.
- Pregnancy complications. Seizures during pregnancy pose dangers to both mother and baby. And certain anti-seizure medicines increase the risk of birth defects. If you have epilepsy and plan to become pregnant, talk with a healthcare professional. Your medicines may need to be adjusted. A healthcare professional likely will monitor your pregnancy.
- Emotional health issues. People with seizures are more likely to have depression and anxiety. Children with seizures may be more likely to develop attention deficit hyperactivity disorder, also called ADHD. Emotional health issues may be a result of dealing with the condition itself or as a result of medicine side effects.
Diagnosis
After a seizure, see a healthcare professional to thoroughly review your symptoms and medical history. You may need several tests to determine the cause of your seizure. The tests can evaluate how likely it is that you'll have another one.
Tests may include:
- Neurological exam. You may have a test of your behavior, ability to move and control your muscles, and ability to think, understand and solve problems. This helps determine if there's a health issue with your brain or other part of your nervous system.
- Blood tests. A blood sample can check for signs of infections, blood sugar levels or electrolyte imbalances.
- Lumbar puncture, also known as a spinal tap. You may need to have a sample of cerebrospinal fluid removed for testing if an infection might have caused the seizure.
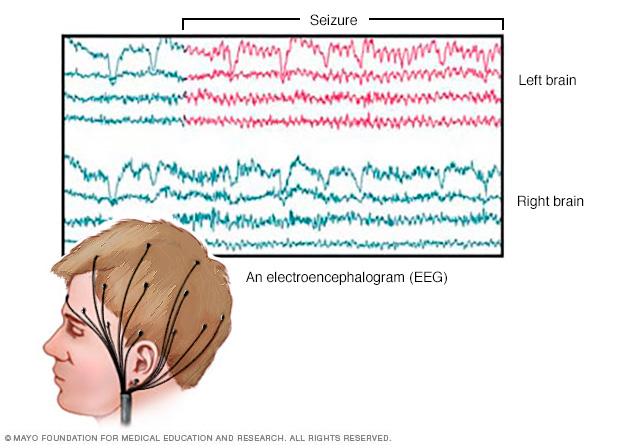
- Electroencephalogram (EEG). In this test, flat metal discs called electrodes attached to your scalp record the electrical activity of your brain. This shows up as wavy lines on an EEG recording. The EEG may reveal a pattern that tells whether a seizure is likely to occur again. EEG testing also may help exclude other conditions that could cause a seizure.
- CT scan. A CT scan uses X-rays to obtain cross-sectional images of your brain. CT scans can reveal tumors, bleeding and cysts in the brain that might cause a seizure.
- MRI. An MRI uses powerful magnets and radio waves to create a detailed view of your brain. An MRI shows the structure of the brain. This can help determine what may be causing the seizures.
- Positron emission tomography (PET). PET scans use a small amount of low-dose radioactive material that's injected into a vein. The material helps visualize active areas of the brain. This can help a healthcare professional see where seizures are occurring.
- Single-photon emission computerized tomography (SPECT). A SPECT test uses a small amount of low-dose radioactive material that's injected into a vein. The test creates a detailed, 3D map of the blood flow activity in your brain that happens during a seizure. You may have a form of a SPECT test called subtraction ictal SPECT coregistered to magnetic resonance imaging, also called SISCOM. This can compare blood flow during a seizure to blood flow in between seizures.
Treatment
Not everyone who has one seizure has another one. Because a seizure can be an isolated incident, you may not start treatment until you've had more than one. Treatment usually involves the use of anti-seizure medicines.
Medications
Many medicines are used in the treatment of epilepsy and seizures. These are usually taken daily by mouth to help prevent seizures. Different medicines may be prescribed based on factors such as your specific seizure type and how often you have them, and your personal considerations such as your age and whether or not you're pregnant.
Finding the right medicine and dosage can be challenging. A healthcare professional likely will prescribe a single medicine at a relatively low dosage, then may increase the dosage gradually until your seizures are well controlled.
Many people with epilepsy are able to prevent seizures with just one medicine. But others need more than one. If you've tried two or more single-drug regimens without success, you may need to try a combination of medicines.
For the best seizure control possible, take medicines exactly as prescribed. Ask a healthcare professional before adding other medicines or stopping your medicine. This includes prescription medicines, medicines available without a prescription or herbal remedies.
Mild side effects of anti-seizure medicines can include:
- Fatigue.
- Dizziness.
- Weight gain.
More-troubling side effects need to be brought to the attention of a healthcare professional right away. They include:
- Mood changes.
- Skin rashes.
- Loss of coordination.
- Speech problems.
- Extreme fatigue.
- Swollen lymph nodes.
- Swelling of the face or eyes, or painful sores in the mouth or around the eyes.
- Trouble swallowing or breathing, including during exercise.
- Discoloration of the skin or eyes such as a yellowing.
- Bruising and bleeding that's not typical.
- Fever and muscle pain.
In rare cases, the medicine lamotrigine has been linked to an increased risk of aseptic meningitis. Aseptic meningitis is an inflammation of the protective membranes that cover the brain and spinal cord. The disease is similar to bacterial meningitis but isn't caused by bacteria.
The U.S. Food and Drug Administration has warned that two anti-seizure medicines can cause a serious reaction, although it happens rarely. Levetiracetam and clobazam can cause inflammation and symptoms that include a rash, fever, swollen lymph nodes, and swelling of the face or eyes. Without quick treatment, the reaction can lead to organ damage, including to the liver, kidneys, lungs, heart or pancreas. It also can lead to death.
These symptoms can begin 2 to 8 weeks after starting levetiracetam or clobazam, but symptoms also may occur earlier or later. Get emergency medical attention if you take these medicines and experience a reaction or any of these serious symptoms.
Talk to your healthcare professional before stopping these medicines. Suddenly stopping the medicines can cause seizures to return.
Surgery and other therapies
When anti-seizure medicines aren't effective, other treatments may be an option:
- Surgery. The goal of surgery is to stop seizures from happening. It may be an option if you have tried two different medicines and they don't prevent your seizures. Surgeons locate and remove the area of your brain where seizures begin. Surgery works best for people who have seizures that originate in the same place in their brains.
- Vagus nerve stimulation. A device placed underneath the skin of your chest stimulates the vagus nerve in your neck. This sends signals to your brain that stop seizures. With vagus nerve stimulation, you may still need to take medicine, but you may be able to lower the dose.
- Responsive neurostimulation. During responsive neurostimulation, a device implanted on the surface of your brain or within brain tissue can detect seizure activity. The device can deliver an electrical stimulation to the detected area to stop the seizure.
- Deep brain stimulation. For this therapy, a surgeon implants electrodes within certain areas of the brain. The electrodes produce electrical impulses that regulate brain activity. The electrodes attach to a pacemaker-like device placed under the skin of your chest. This device controls the amount of stimulation produced.
- Dietary therapy. A diet that's high in fat and protein and low in carbohydrates, known as a ketogenic diet, can improve seizure control. Variations on a ketogenic diet are less effective but may provide benefit. They include the low glycemic index diet and modified Atkins Diet.
Pregnancy and seizures
Women who've had previous seizures usually are able to have healthy pregnancies. Birth defects related to certain medicines can sometimes occur.
In particular, valproic acid has been associated with cognitive deficits and neural tube defects, such as spina bifida. The American Academy of Neurology recommends that women don’t use valproic acid during pregnancy because of risks to the baby.
You may want to talk about these risks with a healthcare professional. Planning before getting pregnant is particularly important for women who've had seizures. In addition to the risk of birth defects, pregnancy can alter medicine levels.
In some cases, it may be appropriate to change the dose of anti-seizure medicine before or during pregnancy. In rare cases, your healthcare professional may consider changing your medicines.
Contraception and anti-seizure medications
It's also important to know that some anti-seizure medicines can make oral contraceptives — a form of birth control — less effective. Also, some oral contraceptives can speed up the metabolism of anti-seizure medicines. Check with a healthcare professional to evaluate whether your medicine interacts with your oral contraceptive. Ask if other forms of contraception need to be considered.

Lifestyle and home remedies
Here are some steps you can take to help with seizure control:
- Take medicine correctly. Don't adjust the dosage before talking to a healthcare professional. Tell the health professional if you feel your medicine should be changed.
- Get enough sleep. Lack of sleep can trigger seizures. Be sure to get adequate rest every night.
- Wear a medical alert bracelet. This helps emergency personnel know how to treat you correctly if you have another seizure.
Personal safety
Seizures don't usually result in serious injury. But injury is possible if you have recurrent seizures. These steps can help you stay safe during a seizure:
- Take care near water. Don't swim alone or ride in a boat without someone nearby.
- Wear a helmet for protection during activities such as bike riding or sports participation.
- Take showers instead of baths unless someone is near you.
- Modify your furnishings. Pad sharp corners, buy furniture with rounded edges and choose chairs that have arms to keep you from falling off the chair. Consider carpet with thick padding to protect you if you fall.
- Display seizure first-aid tips in a place where people can easily see them. Include any important phone numbers there, too.
Seizure first aid
It's helpful to know what to do if you witness someone having a seizure. If you're at risk of having seizures in the future, pass this information along to family, friends and co-workers so that they know what to do.
To help someone during a seizure:
- Carefully roll the person onto one side.
- Place something soft under the person's head.
- Loosen tight clothes from around the neck.
- Remove eyeglasses.
- Don't put your fingers or other objects in the person's mouth.
- Don't try to restrain someone having a seizure.
- Clear away dangerous objects if the person is moving.
- Stay with the person until medical personnel arrive.
- Observe the person closely so that you can provide details on what happened.
- Time the seizure.
- Check for a medical alert bracelet or ID.
- Stay calm.
Coping and support
It can be stressful to live with a seizure disorder. Stress can affect your mental health, so it's important to talk with a healthcare professional about your feelings, who can suggest ways you can find help.
At home
Your family can provide much-needed support. Tell them what you know about your seizure disorder. Let them know they can ask you questions, and be open to conversations about their worries. Help them understand your condition by sharing any educational materials or other resources.
At work
Meet with your supervisor and talk about your seizure disorder and how it affects you. Discuss what you need from your supervisor or co-workers if a seizure happens while at work. Consider talking with your co-workers about seizure disorders. This may help you widen your support system. It also may bring about acceptance and understanding.
You're not alone
Remember, you don't have to go it alone. Reach out to family and friends. Ask your healthcare professional about local support groups or join an online support community. Don't be afraid to ask for help. Having a strong support system is important to living with any medical condition.
Preparing for an appointment
Sometimes seizures need immediate medical attention, and there may not be time to prepare for an appointment.
If your seizure wasn't an emergency, make an appointment with a healthcare professional. You may be referred to a specialist, such as a doctor trained in brain and nervous system conditions, known as a neurologist. Or you may be referred to a neurologist trained in epilepsy, known as an epileptologist.
To prepare for your appointment, consider what you can do to get ready and understand what to expect.
What you can do
- Record information about the seizure. Include the time, location, symptoms you experienced and how long it lasted, if you know these details. Seek input from anyone who may have seen the seizure, such as a family member, friend or co-worker. Record the information they provide.
- Write down any symptoms you or your child has experienced. Include any symptoms that may seem unrelated to the reason for which you scheduled the appointment.
- Make a list of all medicines, vitamins and supplements you're taking. Include the dosages used for each. Also write down the reasons you stopped taking any medicines. Note whether you stopped taking a medicine because of side effects or lack of effectiveness.
- Ask a family member to come with you. It may be hard to remember everything you've been told during your appointment. And since memory loss can happen during seizures, an observer may be able to better describe the seizure.
- Write down your questions.
Preparing a list of questions helps make the most of your time at your appointment. For seizures, some basic questions to ask include:
- Do I have epilepsy?
- Will I have more seizures?
- What kinds of tests do I need? Do these tests require any special preparation?
- What treatments are available and which do you recommend?
- What types of side effects can I expect from treatment?
- Are there any alternatives to the primary approach you're suggesting?
- Is there a generic alternative to the medicine you're prescribing?
- Do I need to restrict any activities?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
Don't hesitate to ask any other questions that occur to you.
What to expect from your doctor
A healthcare professional is likely to ask you a number of questions, such as:
- When did you or your child begin experiencing symptoms?
- How many seizures have you or your child had?
- How often do the seizures occur? How long do they last?
- Can you describe a typical seizure?
- Do the seizures occur in clusters?
- Do they all look the same, or are there different seizure behaviors you or others have noticed?
- What medicines have you or your child tried? What doses were used?
- Have you tried combinations of medicines?
- Have you noticed any seizure triggers, such as sleep deprivation or illness?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


