Overview
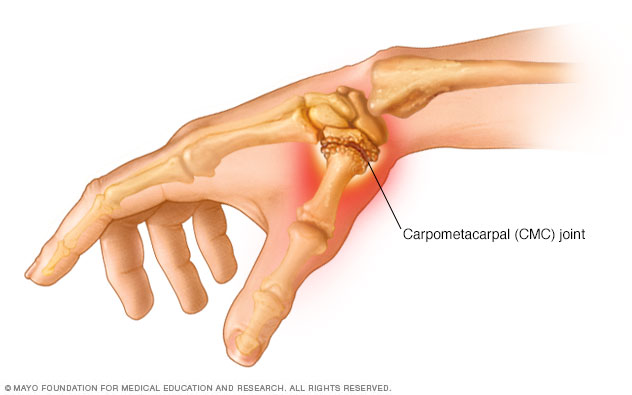
Thumb arthritis is common with aging and occurs when cartilage wears away from the ends of the bones that form the joint at the base of your thumb — also known as the carpometacarpal (CMC) joint.
Thumb arthritis can cause severe pain, swelling, and decreased strength and range of motion, making it difficult to do simple tasks, such as turning doorknobs and opening jars. Treatment generally involves a combination of medication and splints. Severe thumb arthritis might require surgery.
Symptoms
Pain is the first and most common symptom of thumb arthritis. Pain can occur at the base of your thumb when you grip, grasp or pinch an object, or use your thumb to apply force.
Other signs and symptoms might include:
- Swelling, stiffness and tenderness at the base of your thumb
- Decreased strength when pinching or grasping objects
- Decreased range of motion
- Enlarged or bony appearance of the joint at the base of your thumb
When to see a doctor
See your doctor if you have persistent swelling, stiffness or pain at the base of your thumb.
Causes
Thumb arthritis commonly occurs with aging. Previous trauma or injury to the thumb joint also can cause thumb arthritis.
In a normal thumb joint, cartilage covers the ends of the bones — acting as a cushion and allowing the bones to glide smoothly against each other. With thumb arthritis, the cartilage that covers the ends of the bones deteriorates, and its smooth surface roughens. The bones then rub against each other, resulting in friction and joint damage.
The damage to the joint might result in growth of new bone along the sides of the existing bone (bone spurs), which can produce noticeable lumps on your thumb joint.
Risk factors
Factors that can increase your risk of thumb arthritis include:
- Female sex.
- Age above 40 years.
- Obesity.
- Certain hereditary conditions, such as joint ligament laxity and malformed joints.
- Injuries to your thumb joint, such as fractures and sprains.
- Diseases that change the normal structure and function of cartilage, such as rheumatoid arthritis. Although osteoarthritis is the most common cause of thumb arthritis, rheumatoid arthritis can also affect the CMC joint, usually to a lesser extent than other joints of the hand.
- Activities and jobs that put high stress on the thumb joint.
Diagnosis
During a physical exam, your doctor will ask about your symptoms and look for noticeable swelling or lumps on your joints.
Your doctor might hold your joint while moving your thumb, with pressure, against your wrist bone. If this movement produces a grinding sound, or causes pain or a gritty feeling, the cartilage has likely worn down, and the bones are rubbing against each other.
Imaging techniques, usually X-rays, can reveal signs of thumb arthritis, including:
- Bone spurs
- Worn-down cartilage
- Loss of joint space
Treatment
In the early stages of thumb arthritis, treatment usually involves a combination of non-surgical therapies. If your thumb arthritis is severe, surgery might be necessary.
Medication
To relieve pain, your doctor might recommend:
- Topical medications, such as capsaicin or diclofenac, which are applied to the skin over the joint
- Over-the-counter pain relievers, such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve)
- Prescription pain relievers, such as celecoxib (Celebrex) or tramadol (Conzip, Ultram)
Splint
A splint can support your joint and limit the movement of your thumb and wrist. You might wear a splint just at night or throughout the day and night.
Splints can help:
- Decrease pain
- Encourage proper positioning of your joint while you complete tasks
- Rest your joint
Injections
If pain relievers and a splint aren't effective, your doctor might recommend injecting a long-acting corticosteroid into your thumb joint. Corticosteroid injections can offer temporary pain relief and reduce inflammation.
Surgery
If you don't respond to other treatments or if you're barely able to bend and twist your thumb, your doctor might recommend surgery. Options include:
- Joint fusion (arthrodesis). The bones in the affected joint are permanently fused. The fused joint can bear weight without pain, but has no flexibility.
- Osteotomy. The bones in the affected joint are repositioned to help correct deformities.
- Trapeziectomy. One of the bones in your thumb joint (trapezium) is removed.
- Joint replacement (arthroplasty). All or part of the affected joint is removed and replaced with a graft from one of your tendons.
These surgeries can all be done on an outpatient basis. After surgery, you can expect to wear a cast or splint over your thumb and wrist for up to six weeks. Once the cast is removed, you might have physical therapy to help you regain hand strength and movement.
Lifestyle and home remedies
To ease pain and improve joint mobility, try to:
- Modify hand tools. Consider purchasing adaptive equipment — such as jar openers, key turners and large zipper pulls — designed for people with limited hand strength. Replace traditional door handles, which you must grasp with your thumb, with levers.
- Apply cold. Icing the joint for five to 15 minutes several times a day can help relieve swelling and pain.
- Apply heat. For some, heat may be more effective than cold in relieving pain.
Preparing for an appointment
You might be referred to a doctor who specializes in disorders of the joints (rheumatologist).
What you can do
- Write down your symptoms, including any that may seem unrelated to the reason why you scheduled the appointment.
- Write down your key medical information, including other conditions and any history of injury to the painful joint.
- Write down key personal information, including any major changes or stressors in your life.
- Make a list of all your medications, vitamins or supplements.
- Ask a relative or friend to accompany you, to help you remember what the doctor says.
- Write down questions to ask your doctor.
Questions to ask your doctor
- What's the most likely cause of my symptoms?
- What kinds of tests do I need?
- Is my condition likely temporary or chronic?
- What treatments are available?
- Are there any restrictions I should follow?
- I have other health conditions. How can I best manage them together?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may leave time to go over points you want to discuss in depth. You might be asked:
- When did your pain begin?
- How severe are your symptoms? Are they continuous or occasional?
- What, if anything, seems to improve or worsen your symptoms?
- Have you ever injured that hand?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


