Overview
Tetralogy of Fallot (teh-TRAL-uh-jee of fuh-LOW) is a rare heart condition that is present at birth. That means it's a congenital heart defect. A baby born with the condition has four different heart problems.
These heart problems affect the structure of the heart. The condition causes altered blood flow through the heart and to the rest of the body. Babies with tetralogy of Fallot often have blue or gray skin color due to low oxygen levels.
Tetralogy of Fallot is usually diagnosed during pregnancy or soon after a baby is born. If the heart changes and symptoms are mild, tetralogy of Fallot may not be noticed or diagnosed until adulthood.
People who are diagnosed with tetralogy of Fallot need surgery to fix the heart. They will need regular health checkups for life.
Symptoms
Tetralogy of Fallot symptoms depend on how much blood flow is blocked from leaving the heart to go to the lungs. Symptoms may include:
- Blue or gray skin color.
- Shortness of breath and rapid breathing, especially during feeding or exercise.
- Trouble gaining weight.
- Getting tired easily during play or exercise.
- Irritability.
- Crying for long periods of time.
- Fainting.
Tet spells
Some babies with tetralogy of Fallot suddenly develop deep blue or gray skin, nails, and lips. This usually happens when the baby cries, eats or is upset. These episodes are called tet spells.
Tet spells are caused by a rapid drop in the amount of oxygen in the blood. They are most common in young infants, around 2 to 4 months old. Tet spells may be less noticeable in toddlers and older children. That's because they typically squat when they're short of breath. Squatting sends more blood to the lungs.
When to see a doctor
Serious congenital heart defects are often diagnosed before or soon after your child is born. Seek medical help if you notice that your baby has these symptoms:
- Trouble breathing.
- Bluish color of the skin.
- Lack of alertness.
- Seizures.
- Weakness.
- More irritable than usual.
If your baby becomes blue or gray, place your baby on the side and pull the baby's knees up to the chest. This helps increase blood flow to the lungs. Call 911 or your local emergency number immediately.
Causes
Tetralogy of Fallot occurs as the baby's heart grows during pregnancy. Usually, the cause is unknown.
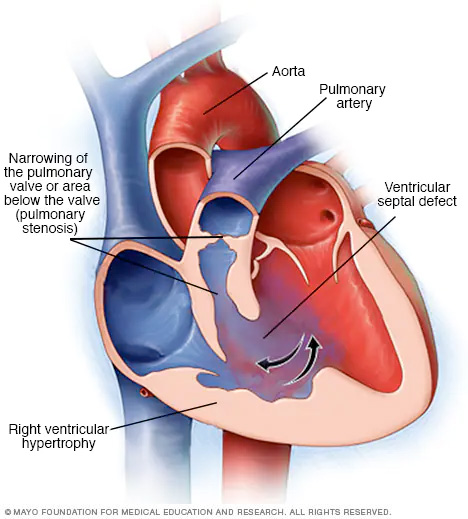
Tetralogy of Fallot includes four problems with heart structure:
- Narrowing of the valve between the heart and the lungs, called pulmonary valve stenosis. This condition reduces blood flow from the heart to the lungs. The narrowing may just involve the valve. Or it could happen in more than one place along the pathway between the heart and lungs. Sometimes the valve isn't formed. Instead, a solid sheet of tissue blocks blood flow from the right side of the heart. This is called pulmonary atresia.
- A hole between the bottom heart chambers, called a ventricular septal defect. A ventricular septal defect changes how blood flows through the heart and lungs. Oxygen-poor blood in the lower right chamber mixes with oxygen-rich blood in the lower left chamber. The heart has to work harder to pump blood through the body. The problem may weaken the heart over time.
- Shifting of the body's main artery. The body's main artery is called the aorta. It's usually attached to the left lower heart chamber. In tetralogy of Fallot, the aorta is in the wrong place. It's shifted to the right and sits directly above the hole in the heart wall. This changes how blood flows from the aorta to the lungs.
- Thickening of the right lower chamber of the heart, called right ventricular hypertrophy. When the heart has to work too hard, the wall of the right lower heart chamber gets thick. Over time, this may cause the heart to become weak and eventually fail.
Some people with tetralogy of Fallot have other problems that affect the aorta or heart arteries. There also may be a hole between the heart's upper chambers, called atrial septal defect.
Risk factors
The exact cause of tetralogy of Fallot is unknown. Some things may increase the risk of a baby being born with tetralogy of Fallot. Risk factors include:
- Family history.
- Having a virus during pregnancy. This includes rubella, also known as German measles.
- Drinking alcohol during pregnancy.
- Eating poorly during pregnancy.
- Smoking during pregnancy.
- Mother's age older than 35.
- Down syndrome or DiGeorge syndrome in the baby.
Complications
Untreated tetralogy of Fallot usually leads to life-threatening complications. The complications may cause disability or death by early adulthood.
A possible complication of tetralogy of Fallot is infection of the inner lining of the heart or heart valves. This is called infective endocarditis. Sometimes antibiotics are given before dental work to prevent this type of infection. Ask your healthcare team if preventive antibiotics are right for you or your baby.
Complications also are possible after surgery to repair tetralogy of Fallot. But most people do well after such surgery. When complications occur, they may include:
- Backward flow of blood through a heart valve.
- Irregular heartbeats.
- A hole in the heart that doesn't go away after surgery.
- Changes in the size of the heart chambers.
- Swelling of part of the aorta, called aortic root dilation.
- Sudden cardiac death.
Another procedure or surgery may be needed to fix these complications.
Congenital heart defects and pregnancy
People born with a complex congenital heart defect may be at risk for complications during pregnancy. Talk to your healthcare team about the possible risks and complications of pregnancy. Together you can discuss and plan for any special care needed.
Prevention
Because the exact cause of most congenital heart defects is unknown, it may not be possible to prevent these conditions. If you have a high risk of giving birth to a child with a congenital heart defect, genetic testing and screening may be done during pregnancy.
There are some steps you can take to help reduce your child's overall risk of birth defects, such as:
- Get proper prenatal care. Regular checkups with a healthcare team during pregnancy can help keep mom and baby healthy.
- Take a multivitamin with folic acid. Taking 400 micrograms of folic acid daily has been shown to reduce birth defects in the brain and spinal cord. It may help reduce the risk of heart defects as well.
- Don't drink or smoke. These lifestyle habits can harm a baby's health. Also avoid secondhand smoke.
- Get a rubella (German measles) vaccine. A rubella infection during pregnancy may affect a baby's heart development. Get vaccinated before trying to get pregnant.
- Control blood sugar. If you have diabetes, good control of your blood sugar can reduce the risk of congenital heart defects.
- Manage chronic health conditions. If you have other health conditions, including phenylketonuria, talk to your healthcare team about the best way to treat and manage them.
- Avoid harmful substances. During pregnancy, have someone else do any painting and cleaning with strong-smelling products.
- Check with your healthcare team before taking any medications. Some medications can cause birth defects. Tell your healthcare team about all the medications you take, including those bought without a prescription.
Diagnosis
Tetralogy of Fallot is often diagnosed soon after birth. Your baby's skin may look blue or gray. A whooshing sound may be heard when listening to the baby's heart with a stethoscope. This is called a heart murmur.
Tests
Tests to diagnose tetralogy of Fallot include:
- Oxygen level measurement. A small sensor placed on a finger or toe quickly checks the amount of oxygen in the blood. This is called a pulse oximetry test.
- Echocardiogram. This test uses sound waves to create pictures of the heart in motion. It shows the heart and heart valves and how well they are working.
- Electrocardiogram, also called ECG or EKG. This test records the electrical activity of the heart. It shows how the heart is beating. Sticky patches called electrodes go on the chest and sometimes the arms or legs. Wires connect the patches to a computer. The computer prints or displays results. An electrocardiogram can help diagnose an irregular heartbeat. Changes in the heart signals also may be due to an enlarged heart.
- Chest X-ray. A chest X-ray shows the shape and condition of the heart and lungs. A common sign of tetralogy of Fallot on an X-ray is a boot-shaped heart. That means the right lower chamber is too big.
- Cardiac catheterization. This test helps to diagnose or treat certain heart conditions. It may be done to plan surgery. The doctor inserts one or more thin, flexible tubes into a blood vessel, usually in the groin. The tubes are called catheters. The doctor guides the tubes to the heart. During the test, doctors can do different heart tests or treatments.
Treatment
All babies who have tetralogy of Fallot need surgery to fix the heart and improve blood flow. A heart surgeon, called a cardiovascular surgeon, does the surgery. The timing and type of surgery depends on the baby's overall health and specific heart problems.
Some babies or young children are given medicine while waiting for surgery to keep blood flowing from the heart to the lungs.
Surgery or other procedures
Surgery used to treat tetralogy of Fallot may include:
-
Temporary surgery, also called temporary repair. Some babies with tetralogy of Fallot need a temporary surgery to improve blood flow to the lungs while waiting for open-heart surgery. This type of treatment is called palliative surgery. A surgeon places a tube called a shunt between a large artery that comes off from the aorta and the lung artery. The tube creates a new path for blood to go to the lungs. This surgery may be done if a baby is born early or if the lung arteries aren't fully developed.
The shunt is removed during open-heart surgery to treat tetralogy of Fallot.
-
Open-heart surgery, called complete repair. People with tetralogy of Fallot need open-heart surgery to completely fix the heart.
A complete repair is usually done in the first year of life. Rarely, a person may not have surgery in childhood if tetralogy of Fallot goes undiagnosed or if surgery is not available. These adults may still benefit from surgery.
A complete repair is done in several steps, The surgeon patches the hole between the lower heart chambers and repairs or replaces the pulmonary valve. The surgeon may remove thickened muscle below the pulmonary valve or widen the smaller lung arteries.
After complete repair, the right lower chamber won't need to work as hard to pump blood. As a result, the right chamber wall should go back to its usual thickness. The oxygen level in the blood goes up. Symptoms typically get better.
Outlook
The long-term survival rates for people who've had tetralogy of Fallot surgery continue to improve.
People with tetralogy of Fallot need lifelong care, preferably from a healthcare team that specializes in heart diseases. The health checkups often include imaging tests to see how well the heart is working. Tests also are done to check for surgery complications.
Lifestyle and home remedies
After treatment for tetralogy of Fallot, your healthcare team may suggest some steps to keep the heart healthy. These may include:
- Sports and activity restrictions. Some people born with a serious heart problem such as tetralogy of Fallot may need to limit exercise or sports activities. But many others can participate in such activities. Ask your or your child's healthcare team which sports and types of activities are safe.
- Antibiotics to prevent heart infection. Sometimes, severe heart problems can increase the risk of infection in the lining of the heart or heart valves. This infection is called endocarditis. Antibiotics may be recommended before dental procedures, especially for people who have a mechanical heart valve. Ask your child's healthcare professional if preventive antibiotics are necessary for your child. Good oral care and regular dental checkups also are important ways to help prevent infection.
Coping and support
You may find that talking with other people who've experienced the same situation brings you comfort and encouragement. Ask your healthcare team if there are any support groups in your area.
Living with a congenital heart problem can make some people feel stressed or anxious. Talking to a therapist or counselor also may help you and your child learn new ways to manage stress and anxiety. Your care team can suggest therapists who may be helpful to you or your child.
Preparing for an appointment
Serious congenital heart problems such as tetralogy of Fallot are typically diagnosed during pregnancy or soon after birth.
If you think your child has a heart problem that wasn't noticed at birth, talk to your child's healthcare team. Be prepared to describe your child's symptoms. Ask family members if anyone was born with a heart problem, called a congenital heart defect. Some congenital heart defects may occur in families.
Here's some information to help you get ready for your appointment.
What you can do
If you have time to prepare for the medical visit, consider taking these steps.
- Make a list of your or your baby's symptoms, including any that seem unrelated to tetralogy of Fallot.
- Write down your or your child's family history, including details from both the mother's and father's family.
- Note any medicines, vitamins or other supplements taken during pregnancy if possible.
- Ask a family member or friend to come with you, if possible. Sometimes it can be difficult to remember all of the information provided to you during an appointment.
- Write down questions to ask the healthcare team.
For tetralogy of Fallot, some basic questions to ask your or your child's doctor include:
- What's the most likely cause of this condition?
- Are there other possible causes of these symptoms?
- What kinds of tests do I or my child need? Do these tests require special preparation?
- What treatments are available, and which do you recommend?
- What are the possible complications of treatment?
- What is the outlook after surgery?
- Are there any activity restrictions?
- Will my child be able to play sports? Can my child participate in gym class?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
You'll usually be asked many questions, such as:
- When did you first notice your child's symptoms?
- Can you describe your child's symptoms?
- When do these symptoms occur?
- Do the symptoms come and go, or does your child always have them?
- Do the symptoms seem to be getting worse?
- Do you have a family history of congenital heart defects?
- Does anything make your child's symptoms better?
- Has your child been growing and meeting developmental milestones as expected? (Ask your child's pediatrician if you're not sure.)
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


