Overview
Spontaneous coronary artery dissection is an emergency condition that occurs when a tear forms in a wall of a heart artery. Spontaneous coronary artery dissection also is called SCAD.
SCAD can slow or block blood flow to the heart, causing a heart attack, heart rhythm problems or sudden death.
SCAD most commonly affects women in their 40s and 50s, though it can occur at any age and can occur in men. People who have SCAD often don't have risk factors for heart disease, such as high blood pressure, high cholesterol or diabetes.
SCAD can cause sudden death if it isn't treated promptly. Get emergency medical help if you have heart attack symptoms — even if you think you aren't at risk of a heart attack.
Symptoms
Symptoms of SCAD can include:
- Chest pain or pressure.
- Pain in the arms, shoulders, back or jaw.
- Shortness of breath.
- Unusual sweating.
- Extreme tiredness.
- Upset stomach.
- A rapid heartbeat or fluttery feeling in the chest.
- Feeling dizzy.
When to see a doctor
Call 911 or your local emergency number if you have chest pain or think you might be having a heart attack. If you don't have access to emergency medical services, have someone drive you to the nearest hospital. Do not drive yourself unless you have no other choice.
Causes
The cause of spontaneous coronary artery dissection is unknown.
Risk factors
Risk factors for SCAD include:
- Being female. SCAD can happen to anyone. But it tends to affect women more than men.
- Childbirth. Some women who have had SCAD have recently given birth. This may be due to changes in hormones and stress on the blood vessels. SCAD has been found to occur most often in the first few weeks after delivery. But SCAD also can occur during pregnancy.
- Extreme stress. SCAD can happen after extreme stress. This includes intense physical exercise and severe emotional distress.
- Fibromuscular dysplasia (FMD). This condition causes weakening of the body's medium-sized arteries. FMD may lead to artery problems such as aneurysm or dissection. Women are more likely to have it than men.
- Genetic conditions affecting connective tissue. Ehlers-Danlos and Marfan syndromes have been found to occur in people who have had SCAD.
- Very high blood pressure. Severe high blood pressure can raise the risk of SCAD.
- Illegal drug use. Using cocaine or other illegal drugs might increase the risk of SCAD.
Complications
A possible complication of SCAD is heart attack. SCAD slows or stops blood flow through an artery. This weakens the heart and may lead to a heart attack. A heart attack from SCAD is different from a heart attack caused by a buildup of fats, cholesterol and other substances in and on the artery walls. This condition is called atherosclerosis.
In some people with SCAD, the inner and outer layers of the artery may split. Blood can collect between these layers. Pressure from the pooled blood can make SCAD worse.
Even with successful treatment, SCAD can happen more than once. It might happen soon after the first episode or years later. People who have SCAD also may have a higher risk of other heart problems. These problems include heart failure due to the heart attack damage.
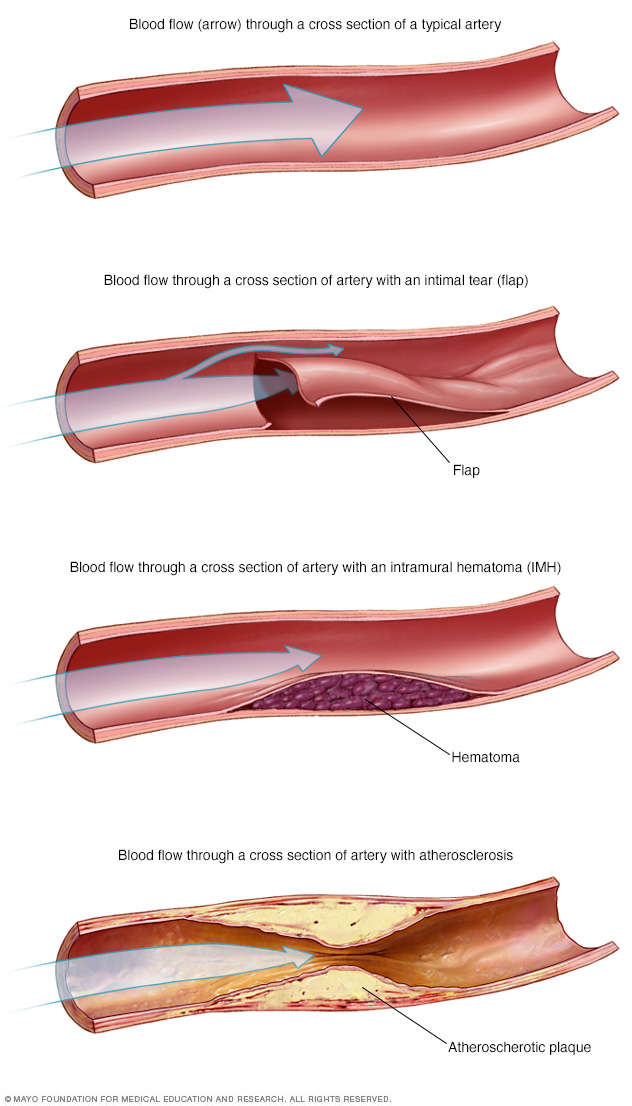 SCAD can reduce or block blood flow through the artery, which can cause a heart attack. A heart attack as a result of SCAD is different from a heart attack caused by atherosclerosis." />
SCAD can reduce or block blood flow through the artery, which can cause a heart attack. A heart attack as a result of SCAD is different from a heart attack caused by atherosclerosis." />Diagnosis
SCAD is usually diagnosed in an emergency setting. You may be asked questions about your personal and family medical history. Tests are done to check your heart.
Tests
Tests to diagnose SCAD are similar to tests used to detect a heart attack. They may include:
- Blood tests. Certain heart proteins slowly leak into the blood after heart damage from a heart attack. Blood tests can check for these proteins. Other blood tests also may be done.
- Electrocardiogram (ECG or EKG). This quick test checks the heart's electrical activity. It can show how fast or how slowly the heart is beating. Sticky patches called electrodes are attached to the chest and sometimes the arms and legs. An electrocardiogram (ECG) can tell if you are having or have had a heart attack.
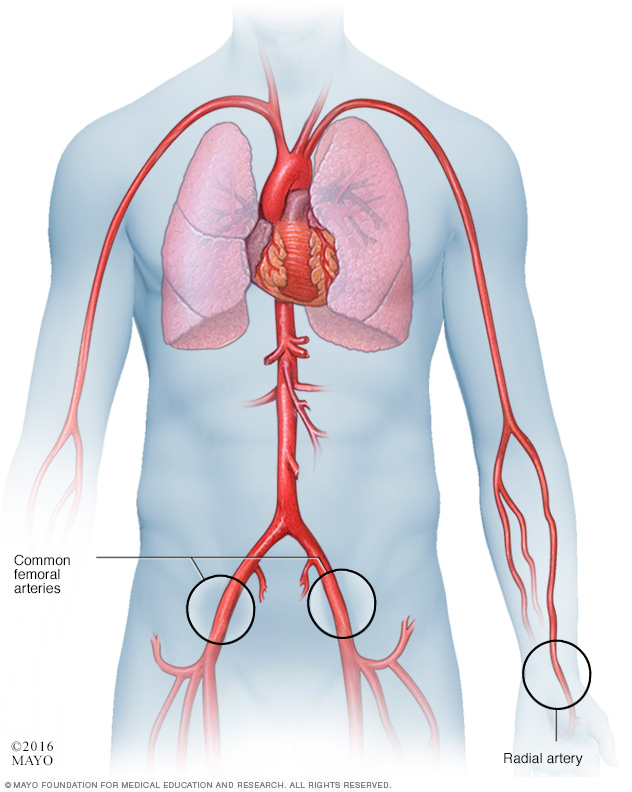
- Coronary angiogram. This test looks inside the heart arteries. A doctor places a long, thin flexible tube called a catheter into a blood vessel, usually in the groin or wrist. It's guided to the heart. Dye flows through the tube to the arteries. The dye helps the arteries show up more clearly on images and video. A coronary angiogram can diagnose SCAD. It also can show any twisted arteries.
Other tests may be done during a coronary angiogram to confirm SCAD and plan treatment. These tests include:
- Optical coherence tomography (OCT). This test uses light to see inside the blood vessels and blood vessel walls. The doctor inserts a flexible tube called a catheter into a blood vessel and guides it to the heart. A beam of light shines from the catheter. The test can help accurately diagnose the cause of a heart attack.
- Intravascular ultrasound (IVUS). Sound waves are used to take pictures of the inside of the heart arteries. The doctor inserts a flexible tube called a catheter into a blood vessel and guides it to the heart. A device on the end of the tube gives off sound waves. A computer looks at the sound waves that bounce back and turns them into pictures of the heart arteries.
Treatment
The goals of SCAD treatment are to:
- Restore blood flow to the heart.
- Manage chest pain.
- Prevent SCAD from happening again.
Treatment may include medicines and a procedure or surgery to open the artery and restore blood flow. Sometimes SCAD heals on its own.
The type of treatment for SCAD depends on your overall health and the size and location of the tear in the artery.
Medications
Some people with SCAD only need medicines to treat symptoms. If chest pain or other symptoms continue, other treatments also might be needed.
Medicines to treat SCAD may include:
- Aspirin. Taking aspirin long-term may help to lower the risk of heart disease after SCAD. Talk to a health care professional to decide if daily aspirin therapy is right for you.
- Blood pressure medicines. Several medicines are available to lower blood pressure. You might need to take these medicines for life to reduce the risk of another SCAD.
- Medicines to control chest pain. Medicines called nitrates and calcium channel blockers can help treat chest pain after SCAD.
Surgery or other procedures
Some people with SCAD need a surgery or procedure to fix the artery and improve blood flow to the heart. These treatments may include:
-
Coronary angioplasty (AN-jee-o-plas-tee) and stent. This treatment may be needed if SCAD blocks blood flow to the heart or medicines don't control chest pain.
During the procedure, a doctor places a long, thin flexible tube called a catheter in a blood vessel, usually in the groin or wrist. It's guided to the heart. A small balloon on the tip of the catheter widens to open the artery. Then, the doctor places a tiny mesh tube called a stent inside the artery. The stent holds the artery open and improves blood flow. The balloon is removed. The stent stays in place. Another name for this treatment is percutaneous coronary intervention or PCI.
- Coronary artery bypass surgery. This open-heart surgery creates a new path for blood to flow around a blocked or partially blocked artery. It may be done if other SCAD treatments don't work or if you have more than one tear. The surgeon takes a healthy blood vessel from the chest or leg area. This healthy vessel is called a graft. One end of the graft is stitched to the artery below the blockage. The other end is stitched to the heart. Other names for this surgery are heart bypass surgery, coronary artery bypass grafting or CABG — pronounced "cabbage."
Pregnancy
If you've had SCAD, talk to a health care professional before becoming pregnant. Pregnancy may not be safe after having SCAD.
Cardiac rehabilitation
After treatment for SCAD, you need regular checkups with your health care team.
A personalized program of exercise and education may be suggested. This is called cardiac rehabilitation, also known as cardiac rehab. It's created to help you recover from a serious heart condition. The program often includes supervised exercise, emotional support and education about a heart-healthy diet.
Lifestyle and home remedies
It's important to take steps to keep the heart healthy. Try these tips:
- Don't smoke. Smoking is a major risk factor for heart disease. Not smoking is the best way to reduce the risk of heart disease and its complications. Also stay away from secondhand smoke. If you need help quitting, ask your care team for strategies that can help.
- Eat healthy foods. Choose whole grains, fruits, vegetables, and lean proteins, such as fish and beans. Avoid or limit foods with a lot of saturated fat, trans fats, salt and sugar.
- Exercise. Regular exercise helps control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. With your provider's OK, aim for 30 to 60 minutes of physical activity most days of the week. Talk to your health care provider about the amount and type of exercise that's best for you. You may be told to avoid intense lifting, competition and extreme temperatures.
- Maintain a healthy weight. Too much weight strains the heart. Being overweight increases the risk of high cholesterol, high blood pressure and diabetes.
- Limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for females and up to two drinks a day for males.
- Control blood pressure, cholesterol and blood sugar. Ask your health care team how often you need to have your blood pressure, blood sugar and cholesterol levels checked.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other health problems. Adults should aim to get 7 to 9 hours of sleep daily. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to a health care professional about strategies that might help.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to ease stress.
Coping and support
Some people might feel scared, sad, frustrated or depressed after having SCAD. Understanding your health and talking to others may help. Try these tips:
- Learn about SCAD. Knowing the details may make you feel more comfortable when talking to your care team. Ask about the size of your artery tear and where it is. Understand the treatments you'll receive and why you need them. Ask where you can find more information.
- Join a support group. It may be helpful to connect with others who know what you're going through. Ask your health care team if there are any SCAD or heart disease support groups in your area.
Preparing for an appointment
You may not have time to prepare. SCAD usually is diagnosed in an emergency situation. If you have chest pain or think that you're having a heart attack, immediately call 911 or your local emergency number.
After a SCAD diagnosis, you may have questions about your health. Prepare a list of questions to ask your health care provider at your next appointment, such as:
- What caused my SCAD?
- What tests do I need?
- What's the most appropriate treatment?
- Will the tear in my artery heal on its own?
- What is my risk of having another SCAD?
- Do I have a blood vessel condition, such as fibromuscular dysplasia, also called FMD?
- I have other health conditions. How can I best manage them together?
- Are there any activity or eating restrictions I need to follow?
- Is it safe for me to get pregnant?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions you have.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


