Overview
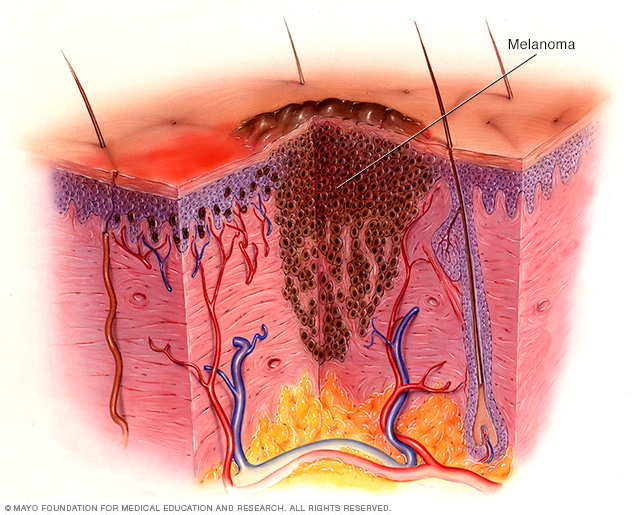
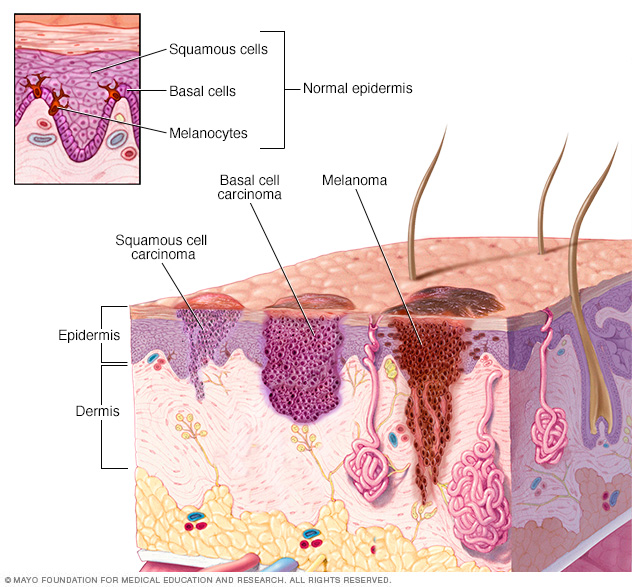
Melanoma is a kind of skin cancer that starts in the melanocytes. Melanocytes are cells that make the pigment that gives skin its color. The pigment is called melanin.
Melanoma typically starts on skin that's often exposed to the sun. This includes the skin on the arms, back, face and legs. Melanoma also can form in the eyes. Rarely, it can happen inside the body, such as in the nose or throat.
The exact cause of all melanomas isn't clear. Most melanomas are caused by exposure to ultraviolet light. Ultraviolet light, also called UV light, comes from sunlight or tanning lamps and beds. Limiting exposure to UV light can help reduce the risk of melanoma.
The risk of melanoma seems to be increasing in people under 40, especially women. Knowing the symptoms of skin cancer can help ensure that cancerous changes are detected and treated before the cancer has spread. Melanoma can be treated successfully if it is found early.
Symptoms
The first melanoma signs and symptoms often are:
- A change in an existing mole.
- The development of a new pigmented or unusual-looking growth on the skin.
Melanoma doesn't always begin as a mole. It also can happen on otherwise healthy skin.
Melanomas symptoms can happen anywhere on the body. Melanomas most often develop in areas that have had exposure to the sun. This includes the arms, back, face and legs.
Melanomas also can happen in areas that aren't as exposed to the sun. This includes the soles of the feet, palms of the hands and fingernail beds. Melanoma also can happen inside the body. These hidden melanomas are more common in people with brown or Black skin.
Typical moles
Typical moles are generally a uniform color. They might look pink, tan, brown or black. In people with brown and Black skin, typical moles are more likely to be dark brown or black. Typical moles have a distinct border separating the mole from the surrounding skin. They're oval or round and usually smaller than 1/4 inch (about 6 millimeters) in diameter.
Most moles begin appearing in childhood and new moles may form until about age 40. By the time they are adults, most people have between 10 and 40 moles. Moles may change in appearance over time and some may even go away with age.
Signs that may indicate melanoma
Some moles aren't typical. They may have certain characteristics that indicate melanomas or other skin cancers. Characteristics may include:
- Asymmetrical shape. Look for moles with unusual shapes, such as two very different-looking halves.
- Changes in color. Look for growths that have many colors or unusual color patterns.
- Changes in size. Look for new growth in a mole larger than 1/4 inch (about 6 millimeters).
- Changes in symptoms. Look for changes in symptoms, such as new itchiness or bleeding.
- Unusual border. Look for moles with unusual, notched or scalloped borders.
Moles that become cancers can all look very different. Some may show all of the changes listed above, while others may have only one or two unusual characteristics.
Hidden melanomas
Melanomas also can develop in areas of the body that have little or no exposure to the sun. These areas may include the spaces between the toes and on the palms, soles, scalp or genitals. These are sometimes referred to as hidden melanomas because they occur in places most people wouldn't think to check. When melanoma occurs in people with brown or Black skin, it's more likely to occur in a hidden area.
Hidden melanomas include:
- Melanoma inside the body. Mucosal melanoma develops in the mucous membrane. This tissue lines the nose, mouth, esophagus, anus, urinary tract and vagina. Mucosal melanomas are especially difficult to detect because they can easily be mistaken for other far more common conditions.
- Melanoma in the eye. Eye melanoma also is called ocular melanoma. It most often occurs in the layer of tissue beneath the white of the eye. This layer is called the uvea. An eye melanoma may cause vision changes and may be diagnosed during an eye exam.
- Melanoma under a nail. Acral-lentiginous melanoma is a rare form of melanoma that can occur under a fingernail or toenail. It also can be found on the palms of the hands or the soles of the feet. Acral-lentiginous melanoma tends to be very dark, flat and have very unusual borders. It's more common in people of Asian descent and people with brown or Black skin.
When to see a doctor
Make an appointment with your doctor or other healthcare professional if you notice any skin changes that worry you.

Causes
Melanoma happens when something changes healthy melanocytes into cancer cells. Melanocytes are skin cells that make pigment that gives skin its color. The pigment is called melanin.
Melanoma starts when melanocytes develop changes in their DNA. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
It isn't clear what changes the DNA in skin cells and how it leads to melanoma. It's likely a combination of factors, including environmental and genetic factors. Still, healthcare professionals believe exposure to ultraviolet light is the leading cause of melanoma. Ultraviolet light, also called UV light, comes from the sun and from tanning lamps and beds.
UV light doesn't cause all melanomas, especially those that occur in places on your body that don't receive exposure to sunlight. This means that other factors may contribute to your risk of melanoma.
Risk factors
Factors that may increase the risk of melanoma include:
- A family history of melanoma. If a close relative has had melanoma, you have a greater chance of developing a melanoma, too. Close relatives may include a parent, child or sibling.
- A history of sunburn. One or more severe, blistering sunburns can increase your risk of melanoma.
- Exposure to UV light. The ultraviolet light, also called UV light, that comes from the sun and from tanning lights and beds increases the risk of skin cancer, including melanoma.
- Having many moles or moles that aren't typical. Having more than 50 typical moles on your body indicates an increased risk of melanoma. Also, having a type of mole that isn't typical increases the risk of melanoma. Known medically as dysplastic nevi, these moles tend to be larger than typical moles. They may have unusual borders and a mixture of colors.
- Living closer to the equator or at a higher elevation. People living closer to the earth's equator experience more direct sun rays. Therefore, they experience higher amounts of UV light from the sun than people living farther north or south. Also, people who live at a higher elevation are more exposed to UV light.
- Skin that sunburns easily. Anyone can get melanoma, but it's most common in people with white skin. If you have blond or red hair, light-colored eyes, and freckle or sunburn easily, you're more likely to develop melanoma.
- Weakened immune system. If the body's germ-fighting immune system is weakened by medications or illness, there might be a higher risk of melanoma and other skin cancers. People with a weakened immune system include those taking medicines to control the immune system, such as after an organ transplant. Certain medical conditions, such as infection with HIV, can weaken the immune system.
Prevention
You can reduce your risk of melanoma and other types of skin cancer if you:
- Avoid tanning lamps and beds. Tanning lamps and beds give off ultraviolet light, also called UV light. Exposure to this kind of light can increase your risk of skin cancer.
- Avoid the sun during the middle of the day. For many people in North America, the sun's rays are strongest between about 10 a.m. and 4 p.m. Schedule outdoor activities for other times of the day, even in winter or when the sky is cloudy.
-
Become familiar with your skin so that you'll notice changes. Check your skin often for new skin growths. Look for changes in existing moles, freckles, bumps and birthmarks. With the help of mirrors, check your face, neck, ears and scalp.
Look at your chest and trunk and the tops and undersides of your arms and hands. Check both the front and back of your legs and your feet, including the soles and the spaces between your toes. Also check your genital area and between your buttocks.
-
Wear protective clothing. When you go outside during the day, wear clothes that help protect your skin from the sun's rays. Cover your skin with dark, tightly woven clothing that covers your arms and legs. Wear a broad-brimmed hat, which provides more protection than does a baseball cap or visor. Some companies also sell protective clothing. A dermatologist can recommend an appropriate brand.
Don't forget sunglasses. Look for those that block both types of UV light that come from the sun, called UVA and UVB.
- Wear sunscreen year-round. Use a broad-spectrum sunscreen with an SPF of at least 30, even on cloudy days. Apply sunscreen generously. Reapply every two hours, or more often if you're swimming or sweating.
Diagnosis
Tests and procedures used to diagnose melanoma include:
Physical exam
Your healthcare professional will ask questions about your health history. That person also will examine your skin to look for signs that could mean melanoma.
Removing a sample of tissue for testing
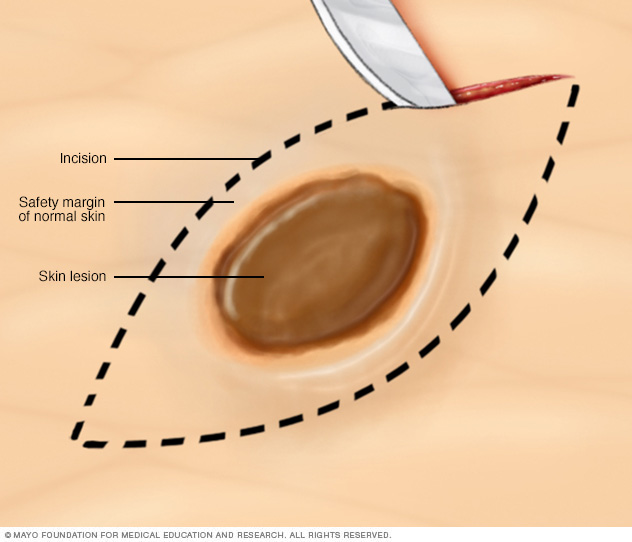
A biopsy is a procedure to remove a sample of tissue for testing in a lab. What type of biopsy procedure is used depends on your situation. Most often healthcare professionals recommend removing the entire growth when possible.
One common technique is called the punch biopsy. A punch biopsy is done with a circular blade that's pressed into the skin around the suspicious mole.
Another technique is called an excisional biopsy. An excisional biopsy uses a scalpel to cut away the entire mole and some of the healthy tissue around it.
Determining the extent of the melanoma
If you receive a diagnosis of melanoma, the next step is to determine the extent of the cancer, called the stage. To assign a stage to your melanoma, your healthcare team will:
-
Determine the thickness. In general, the thicker the melanoma, the more serious the disease. The thickness of a melanoma is determined by looking at the melanoma under a microscope and measuring it with a special tool. The thickness of a melanoma helps your care team decide on a treatment plan.
Thinner melanomas may only require surgery to remove the cancer and some healthy tissue around it. If the melanoma is thicker, your healthcare team may recommend more tests to see if the cancer has spread before deciding on your treatment options.
-
See if the melanoma has spread to the lymph nodes. If there's a risk that the cancer has spread to nearby lymph nodes, you might need a sentinel node biopsy.
During a sentinel node biopsy, a dye is injected in the area where your melanoma was removed. The dye flows to the nearby lymph nodes. The first lymph nodes to take up the dye are removed and tested for cancer cells. These first lymph nodes are called the sentinel lymph nodes. If they're cancer-free, there's a good chance that the melanoma has not spread.
- Look for signs of cancer beyond the skin. If there is concern that the melanoma has spread, imaging tests might be used to look for signs of cancer in other areas of the body. Tests might include X-ray, MRI, CT and positron emission tomography, which is also called a PET scan. These imaging tests generally aren't used for smaller melanomas with a lower risk of spreading beyond the skin.
Other factors may go into determining the risk that the cancer may spread. One factor is whether the skin over the area has formed an open sore, called ulceration. Another is how many dividing cancer cells are found when looking at a sample of the cancer under a microscope. Doctors call this the cancer's mitotic rate.
Your healthcare team uses the results from these tests to figure out your melanoma's stage. Melanoma stages use the numbers 0 through 4. At stage 0 and stage 1, a melanoma is thin and small. Treatment is likely to be successful. As the melanoma grows deeper into the skin, the stages get higher. Treatment becomes more challenging. By stage 4, the cancer has spread beyond the skin to other organs, such as the lungs or liver.
Treatment
Melanoma treatment often starts with surgery to remove the cancer. Other treatments may include radiation therapy and treatment with medicine. Treatment for melanoma depends on several factors. These factors include the stage of your cancer, your overall health and your own preferences.
Surgery
Treatment for melanoma usually includes surgery to remove the melanoma. A very thin melanoma may be removed entirely during the biopsy and require no further treatment. Otherwise, your surgeon will remove the cancer as well as some of the healthy tissue around it.
For people with melanomas that are small and thin, surgery might be the only treatment needed. If the melanoma has grown deeper into the skin, there might be a risk that the cancer has spread. So other treatments are often used to make sure all the cancer cells are killed.
If the melanoma has grown deeper into the skin or if it may have spread to the nearby lymph nodes, surgery might be used to remove the lymph nodes.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body.
Radiation therapy may be directed to the lymph nodes if the melanoma has spread there. Radiation therapy also can be used to treat melanomas that can't be removed completely with surgery. For melanoma that spreads to other areas of the body, radiation therapy can help relieve symptoms.
Immunotherapy
Immunotherapy for cancer is a treatment with medicine that helps the body's immune system to kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
For melanoma, immunotherapy may be used after surgery for cancer that has spread to the lymph nodes or to other areas of the body. When melanoma can't be removed completely with surgery, immunotherapy treatments might be injected directly into the melanoma.
Targeted therapy
Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
For melanoma, targeted therapy might be recommended if the cancer has spread to your lymph nodes or to other areas of your body. Cells from your melanoma may be tested to see if targeted therapy is likely to be effective against your cancer.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Most are given through a vein. Some come in pill form.
Chemotherapy might be an option to help control melanoma that doesn't respond to other treatments. It might be used when immunotherapy or targeted therapy aren't helping.
Sometimes chemotherapy can be given in a vein in your arm or leg in a procedure called isolated limb perfusion. During this procedure, blood in your arm or leg isn't allowed to travel to other areas of your body for a short time. This helps keep the chemotherapy medicines near the melanoma and doesn't affect other parts of your body.
Coping and support
With time, you'll find what helps you cope with the uncertainty and distress of a cancer diagnosis. Until then, you may find it helps to:
Learn enough about melanoma to make decisions about your care
Ask your healthcare team about your cancer, including your test results, treatment options and, if you like, your prognosis. As you learn more about melanoma, you may become more confident in making treatment decisions.
Keep friends and family close
Keeping your close relationships strong will help you deal with your melanoma. Friends and family can provide the practical support you'll need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by having cancer.
Find someone to talk with
Find someone who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area. Other sources of information include the National Cancer Institute and the American Cancer Society.
Preparing for an appointment
Make an appointment with a doctor or other healthcare professional if you notice any skin changes that worry you.
If your healthcare professional thinks you might have melanoma, you may be referred to a doctor who specializes in skin diseases. This doctor is called a dermatologist. If a cancer diagnosis is made, you also may be referred to a doctor who specializes in treating cancer. This doctor is called an oncologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you're experiencing, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down key personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so prepare a list of questions to help you make the most of your time together. List your questions from most important to least important in case time runs out. For melanoma, some basic questions to ask include:
- Do I have melanoma?
- How large is my melanoma?
- How deep is my melanoma?
- Has my melanoma spread beyond the area of skin where it was first discovered?
- What additional tests do I need?
- What are my treatment options?
- Can any treatment cure my melanoma?
- What are the potential side effects of each treatment option?
- Is there one treatment you feel is best for me?
- How long can I take to decide on a treatment option?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
Don't hesitate to ask other questions.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


