Overview
Cholesterol is a waxy substance found in the blood. The body needs cholesterol to build healthy cells. But high levels of cholesterol can raise the risk of heart disease.
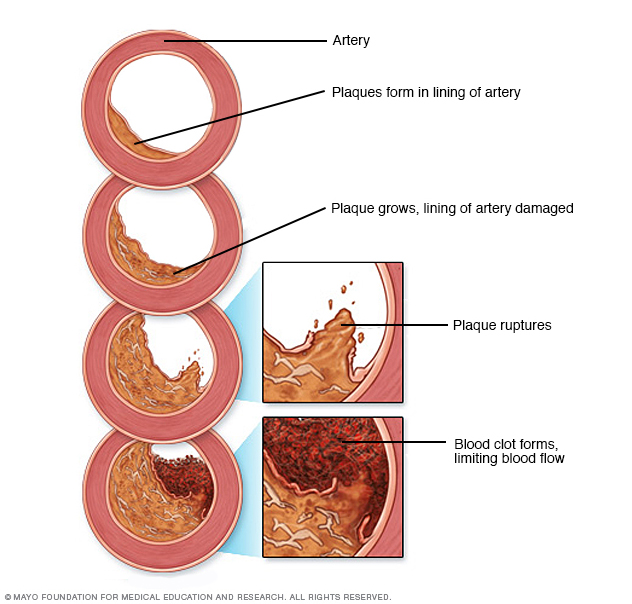
With high cholesterol, fats and other substances can build up in blood vessels called arteries. This buildup is called plaque. As more plaque forms over time, the arteries can become narrowed or clogged. That makes it hard for enough blood to flow through the arteries. Sometimes a piece of plaque can break loose and form a blood clot. The clot may cause a heart attack or stroke.
High cholesterol can be inherited. That means it can pass from parents to children through genes. But high cholesterol often is the result of lifestyle choices such as not getting enough exercise, not eating a balanced diet or consuming large amounts of saturated fat. You can make changes to help prevent it. And if you have high cholesterol, you can help lower it with a healthy diet, regular exercise and sometimes medicine.
Symptoms
High cholesterol has no symptoms. A blood test is the only way to find out if you have it.
When to see a doctor
The American Heart Association recommends that children get checked, also called screened, for high cholesterol once between ages 9 and 11. Screening may start earlier if a child has a family history of high cholesterol, heart attack or stroke. Screening also may start earlier if a child has conditions such as diabetes or obesity.
The next cholesterol screening is recommended for people between ages 17 and 21. After that, many adults get their cholesterol checked every 4 to 6 years. People who have health conditions such as high blood pressure and diabetes may need to get screened more often. So might those who take cholesterol-lowering medicine. Those who have a family history of high cholesterol or heart disease also may need more-frequent screenings.
If your test results aren't within the desirable range, your healthcare professional might recommend more-frequent testing as well.
Causes
Lifestyle factors that may be within your control are the most common cause of high cholesterol. These factors include eating a diet high in saturated and trans fats and not getting enough exercise.
Sometimes factors that aren't within your control can lead to high cholesterol. These include gene changes that pass from parents to children, some health conditions, and some medicines.
Conditions that can cause high cholesterol include:
- Familial hypercholesterolemia.
- Chronic kidney disease.
- Chronic liver disease.
- Diabetes.
- HIV/AIDS.
- Hypothyroidism.
- Lupus.
- Overweight and obesity.
- Sleep apnea.
Some types of medicines taken for other health conditions also can make cholesterol levels worse. These include treatments for:
- Acne.
- Cancer.
- High blood pressure.
- HIV/AIDS.
- Irregular heartbeats.
- Organ transplants.
Cholesterol travels through the blood, attached to proteins. This mix of proteins and cholesterol is called a lipoprotein. There are various types of cholesterol. The types are based on what the lipoprotein carries. They are:
-
Low-density lipoprotein (LDL) cholesterol. This is known as the "bad" cholesterol. LDL carries cholesterol particles throughout the body. "Bad" cholesterol builds up in the walls of arteries. This makes the arteries hard and narrow.
When a gene change causes high cholesterol, the body has trouble removing LDL cholesterol from the blood. Or the body has trouble breaking down LDL cholesterol in the liver.
- High-density lipoprotein (HDL) cholesterol. This is known as the "good" cholesterol. HDL picks up extra cholesterol and takes it back to the liver.
Most often, a blood test to check cholesterol levels also measures a type of fat in the blood that is not a type of cholesterol, called triglycerides. Having a high triglyceride level also can raise the risk of heart disease. Lifestyle factors that you may be able to control play a role in triglyceride levels.
Risk factors
Risk factors for high cholesterol levels include:
- Eating habits. Eating too much saturated fat or trans fats can lead to high cholesterol. Saturated fats are found in fatty cuts of meat and full-fat dairy products. Sometimes trans fats are found in packaged snacks or desserts.
- Obesity. This complex disease involves having too much body fat.
- Lack of exercise. Exercise helps boost the body's "good" HDL cholesterol.
- Smoking. Cigarette smoking may lower the level of HDL.
- Alcohol. Drinking lots of alcohol can raise total cholesterol. Try to limit alcohol to up to one drink a day for women and up to two drinks a day for men.
- Age. Even young children can have high cholesterol. But it's much more common in people over 40. As you age, your liver becomes less able to remove "bad" LDL cholesterol.
Complications
High cholesterol can lead to other health conditions called complications. With high cholesterol, a dangerous amount of plaque can build up on the walls of arteries. This is called atherosclerosis. Over time, the plaque buildup can cause arteries to narrow and block blood flow. Less blood flow through the arteries can cause complications such as:
- Chest pain, also called angina. If the arteries that supply the heart with blood are affected, that may cause chest pain. It also may cause other symptoms of a common type of heart disease called coronary artery disease.
- Heart attack. If plaques tear or break, a blood clot can form. The clot may block the flow of blood at the site where it broke. Or it may completely break free and block an artery farther away. If blood flow to part of the heart stops, a heart attack happens. A heart attack is an emergency that needs treatment right away.
- Stroke. A stroke happens when a blood clot blocks blood flow to part of the brain. It's also an emergency that needs treatment right away.
Prevention
The same heart-healthy lifestyle changes that can lower cholesterol also can help prevent high cholesterol. You can practice the following habits:
- Eat a diet that focuses on lean protein, fruits, vegetables and whole grains. Limit sodium and added sugar.
- Also limit the amount of saturated and trans fats you eat. Instead, eat foods with healthy fats such as fatty or oily fish, nuts, and olive or canola oil.
- Lose extra weight and keep it off.
- If you smoke, ask your care team to help you quit.
- Exercise on most days of the week for at least 30 minutes.
- Drink less alcohol, if at all. Limit alcohol to no more than up to one drink a day for women and up to two drinks a day for men.
Diagnosis
Diagnosis involves the steps that your healthcare professional takes to find out if you have high cholesterol. You receive a blood test to check cholesterol levels. You might hear the blood test called a lipid panel or a lipid profile. The results of the test usually show your:
- Total cholesterol.
- Low-density lipoprotein (LDL) cholesterol.
- High-density lipoprotein (HDL) cholesterol.
- Triglycerides.
In general, you can't have food or liquids other than water for around 9 to 12 hours before the test. This is called fasting. Some cholesterol tests don't require fasting, so follow your healthcare professional's instructions.
Interpreting the numbers
In the United States, cholesterol levels are measured in milligrams (mg) of cholesterol per deciliter (dL) of blood. In Canada and many European countries, cholesterol levels are measured in millimoles per liter (mmol/L). To interpret your test results, use these general guidelines.
| Total cholesterol (U.S. and some other countries) | Total cholesterol* (Canada and most of Europe) | Results |
|---|---|---|
| *Canadian and European guidelines differ slightly from U.S. guidelines. These conversions are based on U.S. guidelines. | ||
| Below 200 mg/dL | Below 5.2 mmol/L | Desirable |
| 200-239 mg/dL | 5.2-6.2 mmol/L | Borderline high |
| 240 mg/dL and above | Above 6.2 mmol/L | High |
| LDL cholesterol (U.S. and some other countries) | LDL cholesterol* (Canada and most of Europe) | Results |
|---|---|---|
| *Canadian and European guidelines differ slightly from U.S. guidelines. These conversions are based on U.S. guidelines. | ||
| Below 70 mg/dL | Below 1.8 mmol/L | Desirable for people who have coronary artery disease or other forms of atherosclerosis. Optimal for people at high risk or very high risk of coronary artery disease or other forms of atherosclerosis. In some people the desired value could be below 55 mg/dL. |
| Below 100 mg/dL | Below 2.6 mmol/L | Optimal for healthy people without coronary artery disease or other forms of atherosclerosis. |
| 100-129 mg/dL | 2.6-3.3 mmol/L | Near optimal for people who do not have coronary artery disease or other forms of atherosclerosis. High if there is coronary artery disease or other forms of atherosclerosis. |
| 130-159 mg/dL | 3.4-4.1 mmol/L | Borderline high for people who do not have coronary artery disease or other forms of atherosclerosis. High if there is coronary artery disease or other forms of atherosclerosis. |
| 160-189 mg/dL | 4.1-4.9 mmol/L | High for people who do not have coronary artery disease. Very high if there is coronary artery disease or other forms of atherosclerosis. |
| 190 mg/dL and above | Above 4.9 mmol/L | Very high. |
| HDL cholesterol (U.S. and some other countries) | HDL cholesterol* (Canada and most of Europe) | Results |
|---|---|---|
| *Canadian and European guidelines differ slightly from U.S. guidelines. These conversions are based on U.S. guidelines. | ||
| Below 40 mg/dL, men | Below 1.0 mmol/L, men | Low |
| Below 50 mg/dL, women | Below 1.3 mmol/L, women | |
| 40-59 mg/dL, men | 1-1.5 mmol/L, men | Better |
| 50-59 mg/dL, women | 1.3-1.5 mmol/L, women | |
| 60 mg/dL and above | Above 1.5 mmol/L | Best |
| Triglycerides (U.S. and some other countries) | Triglycerides* (Canada and most of Europe) | Results |
|---|---|---|
| *Canadian and European guidelines differ slightly from U.S. guidelines. These conversions are based on U.S. guidelines. | ||
| Below 150 mg/dL | Below 1.7 mmol/L | Desirable |
| 150-199 mg/dL | 1.7-2.2 mmol/L | Borderline high |
| 200-499 mg/dL | 2.3-5.6 mmol/L | High |
| 500 mg/dL and above | Above 5.6 mmol/L | Very high |
Children and cholesterol testing
The American Heart Association recommends that children get checked, also called screened, for high cholesterol once between ages 9 and 11. Screening may start earlier if a child has a family history of high cholesterol, heart attack or stroke. Screening also may start earlier if a child has conditions such as diabetes or obesity. The next cholesterol screening is recommended between ages 17 and 21.
Treatment
Treatment choices to reach ideal cholesterol and triglyceride levels should be tailored to meet your needs. Talk with your healthcare professional about what levels are best for you.
Treatment for high cholesterol can include medicine. Together with healthy lifestyle changes, medicine can lower the risk of heart attacks and strokes.
You may benefit from one or more medicines. It depends on things such as your risk factors, age, health and possible medicine side effects. Your healthcare professional helps choose the right treatments for you.
Common cholesterol medicines include:
Statins
Statins block a substance that the liver needs to make cholesterol. This causes the liver to make less cholesterol and to remove cholesterol from the blood.
Statin choices include:
- Atorvastatin (Lipitor).
- Fluvastatin (Lescol XL).
- Lovastatin (Altoprev).
- Pitavastatin (Livalo, Zypitamag).
- Pravastatin.
- Rosuvastatin (Crestor).
- Simvastatin (Zocor).
Cholesterol absorption inhibitors
The small intestine absorbs the cholesterol from food and releases it into the bloodstream. The medicine ezetimibe (Zetia) helps lower the amount of cholesterol absorbed from food. Your healthcare professional may prescribe ezetimibe with a statin.
Bempedoic acid
Bempedoic acid (Nexletol) works in much the same way as statins. Your healthcare professional may prescribe it if statins cause serious side effects for you. Adding bempedoic acid to a statin can help lower LDL. A pill that contains both bempedoic acid and ezetimibe, called Nexlizet, also is available.
Bile acid sequestrants
The liver uses cholesterol to make bile acids. The body needs these substances for digestion. Bile acid sequestrants bind to bile acids. This prompts the liver to use extra cholesterol to make more bile acids. In turn, that lowers the level of cholesterol in the blood.
Bile acid sequestrants include cholestyramine (Prevalite), colesevelam (Welchol) and colestipol (Colestid).
PCSK9 inhibitors
These medicines can help the liver absorb more LDL cholesterol. This lowers the amount of cholesterol in the blood. Alirocumab (Praluent), evolocumab (Repatha) or inclisiran (Leqvio) might be used for people who have a genetic condition that causes very high levels of LDL. These medicines also may be used in people with a history of heart disease when statins or other cholesterol medicines don’t do enough to lower cholesterol levels. PCSK9 inhibitors are given as a shot under the skin.
Medicines for high triglycerides
If you also have high triglycerides, your healthcare professional may prescribe:
- Fibrates. The medicines fenofibrate (Lipofen) and gemfibrozil (Lopid) speed the removal of triglycerides from the blood. They also help lower LDL cholesterol. Using a fibrate with a statin can raise the risk of statin side effects.
- Niacin. Niacin limits the liver's ability to make LDL cholesterol. But niacin doesn't provide more benefits than a statin. Niacin also has been linked with liver damage and strokes. Most healthcare professionals now recommend it only for people who can't take statins.
- Omega-3 fatty acids. Omega-3 fatty acids can help lower triglycerides. They are available with or without a prescription. If you choose to take supplements without a prescription, talk with your healthcare professional first. Omega-3 fatty acids may affect other medicines that you take. The effectiveness and cost of omega-3 fatty acids varies.
Medicine side effects
Let your healthcare professional know if your cholesterol medicine causes side effects. For instance, side effects of statins can include:
- Muscle pains.
- Muscle damage (very rare).
- Increased blood sugar.
If you decide to take cholesterol medicine, your healthcare professional may recommend liver function tests. These tests help check the medicine's effect on your liver.
Children and cholesterol treatment
Most often, making changes to diet and exercise is the first treatment for children age 2 and older who have high cholesterol. Children age 10 and older who have very high cholesterol levels might be prescribed cholesterol-lowering drugs such as statins.
Lifestyle and home remedies
Lifestyle changes are important if you have high cholesterol. Try to make the following healthy changes:
- Lose extra weight. Losing weight can help lower cholesterol.
- Eat a heart-healthy diet. Focus on plant-based foods. These include fruits, vegetables and whole grains. Limit added sugar and sodium. Also limit saturated fats and trans fats. Healthy fat, found in olive and canola oils, is a better option. Avocados, nuts and oily fish are other sources of healthy fat.
- Be active in your daily life and exercise regularly. Talk with your healthcare professional if you're not active already. Work up to at least 30 minutes of exercise five times a week.
- Don't smoke. If you smoke, you can ask your healthcare professional to help you quit.
- Limit alcohol or don't drink it. Limit alcohol to no more than up to one drink a day for women and up to two for men.
- Manage stress. Activities such as exercise and meditation can help.
- Get enough sleep. It's ideal for adults to get about 7 to 9 hours of sleep each night.
Preparing for an appointment
If you're an adult who hasn't had regular cholesterol level checks, make an appointment with your healthcare professional. Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance. For a cholesterol test, you'll likely have to stop eating and drinking about 9 to 12 hours before the test. You may be able to have water if your healthcare team says it's OK.
Make a list of:
- Your symptoms, if any.
- Key personal information, including a family history of high cholesterol, coronary artery disease, strokes, high blood pressure or diabetes.
- All medicines, vitamins or supplements you take, including doses.
- Questions to ask your healthcare professional.
For high cholesterol, some basic questions to ask your healthcare professional include:
- What tests do I need?
- What's the best treatment?
- How often do I need a cholesterol test?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Feel free to ask other questions.
What to expect from your doctor
Your healthcare team is likely to ask you questions such as:
- What's your diet like?
- How much exercise do you get?
- How much alcohol do you drink?
- Do you smoke? Are you or were you around other smokers?
- When was your last cholesterol test? What were the results?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


