Overview
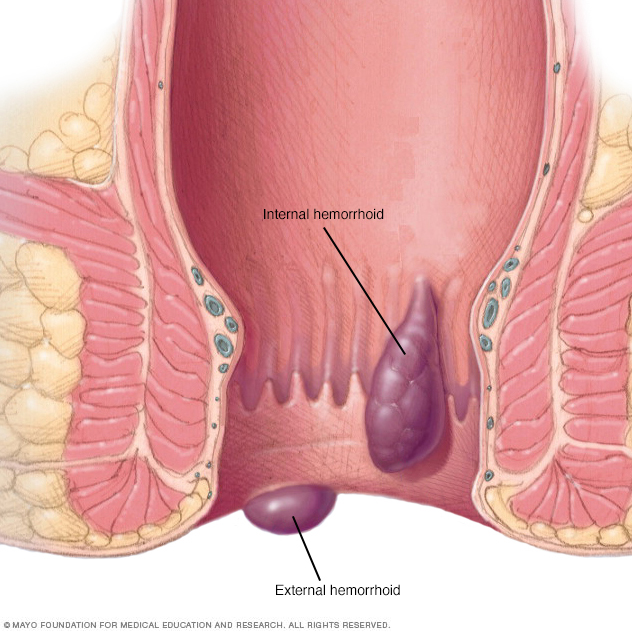
Hemorrhoids (HEM-uh-roids), also called piles, are swollen veins in the anus and lower rectum. Hemorrhoids are similar to varicose veins. Hemorrhoids can develop inside the rectum, called internal hemorrhoids. They also can develop under the skin around the anus, called external hemorrhoids.
There are several options available to treat hemorrhoids. Many people get relief with home treatments and lifestyle changes.
Symptoms
Symptoms of hemorrhoids usually depend on the type of hemorrhoid.
Internal hemorrhoids
Internal hemorrhoids lie inside the rectum. You usually can't see or feel them, and they rarely cause discomfort. But straining or irritation when passing stool can cause:
- Painless bleeding during bowel movements. You might notice small amounts of bright red blood on your toilet tissue or in the toilet.
- A hemorrhoid to push through the anal opening, called a prolapsed or protruding hemorrhoid. This may result in pain and irritation.
External hemorrhoids
These are under the skin around the anus. Symptoms might include:
- Itching or irritation in the anal region.
- Pain or discomfort.
- Swelling around the anus.
- Bleeding.
Thrombosed hemorrhoids
Blood can pool in an external hemorrhoid and form a clot, called a thrombus. A thrombosed hemorrhoid can result in:
- Severe pain.
- Swelling.
- Inflammation.
- A hard, discolored lump near the anus.
When to see a doctor
If you have bleeding during bowel movements or you have hemorrhoids that don't improve after a week of home care, talk to your health care provider.
Don't assume rectal bleeding is due to hemorrhoids, especially if you have changes in bowel habits or if your stools change in color or consistency. Rectal bleeding can happen with other diseases, including colorectal cancer and anal cancer.
Seek emergency care if you have large amounts of rectal bleeding, lightheadedness, dizziness or faintness.
Causes
The veins around the anus tend to stretch under pressure and may bulge or swell. Hemorrhoids can develop from increased pressure in the lower rectum due to:
- Straining during bowel movements.
- Sitting for long periods of time, especially on the toilet.
- Having chronic diarrhea or constipation.
- Being obese.
- Being pregnant.
- Having anal intercourse.
- Eating a low-fiber diet.
- Regularly lifting heavy items.
Risk factors
As people age, the risk of hemorrhoids increases. That's because the tissues that support the veins in the rectum and anus can weaken and stretch. This also can happen during pregnancy because the baby's weight puts pressure on the anal region.
Complications
Complications of hemorrhoids are rare but may include:
- Anemia. Rarely, ongoing blood loss from hemorrhoids may cause anemia. Anemia is when there aren't enough healthy red blood cells to carry oxygen to the body's cells.
- Strangulated hemorrhoid. When the blood supply to an internal hemorrhoid is cut off, the hemorrhoid is called strangulated. Strangulated hemorrhoids can cause extreme pain.
- Blood clot. Sometimes a clot can form in a hemorrhoid. This is called a thrombosed hemorrhoid. Although not dangerous, it can be extremely painful and sometimes needs to be drained.
Prevention
The best way to prevent hemorrhoids is to keep your stools soft so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk. This will help you avoid the straining that can cause hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Drink plenty of fluids. Drink 6 to 8 glasses of water and other liquids each day to help keep stools soft. Avoiding alcohol also may help.
-
Consider fiber supplements. Most people don't get enough fiber in their diets. Studies have shown that nonprescription fiber supplements, such as psyllium (Metamucil, Konsyl, others) or methylcellulose (Citrucel), can lessen symptoms and bleeding from hemorrhoids.
If you use fiber supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause constipation or make it worse.
- Don't strain. Straining and holding your breath when trying to pass stool create greater pressure in the veins in the lower rectum.
- Exercise. Stay active to help prevent constipation and reduce pressure on veins. Exercise also can help you lose excess weight that might be causing your hemorrhoids or making them worse.
- Avoid long periods of sitting. Sitting too long, especially on the toilet, can increase the pressure on the veins in the anus.
Diagnosis
Your health care provider might be able to see external hemorrhoids. Diagnosing internal hemorrhoids might include an exam of your anal canal and rectum.
- Digital examination. Your health care provider inserts a gloved, lubricated finger into your rectum. This allows your provider to check for anything unusual, such as growths.
- Visual inspection. Internal hemorrhoids are often too soft to be felt during a rectal exam. Your health care provider might look at the lower part of your colon and rectum with a tool such as an anoscope, a proctoscope or a sigmoidoscope.
Your health care provider might want to look at your entire colon using colonoscopy if:
- Your symptoms suggest you might have another digestive system disease.
- You have risk factors for colorectal cancer.
- You are middle aged and haven't had a recent colonoscopy.
Treatment
Home remedies
You can often relieve the mild pain, swelling and inflammation of hemorrhoids with home treatments.
- Eat high-fiber foods. Eat more foods that are high in fiber. This helps softens the stool and increases its bulk, which will help you avoid straining. Add fiber to your diet slowly to avoid problems with gas.
- Use topical treatments. Apply a hemorrhoid cream or suppository containing hydrocortisone that you can buy without a prescription. You also can use pads containing witch hazel or a numbing medicine.
- Soak regularly in a warm bath or sitz bath. Soak your anal area in plain warm water for 10 to 15 minutes two or three times a day. A sitz bath fits over the toilet.
- Take pain relievers by mouth. You can temporarily use acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others) to help relieve your discomfort.
With these treatments, hemorrhoid symptoms often go away within a week. See your health care provider within a week if you don't get relief. Contact your provider sooner if you have severe pain or bleeding.
Medicines
Your hemorrhoids might only produce mild discomfort. In this case, your health care provider may suggest creams, ointments, suppositories or pads that you can buy without a prescription. These products contain ingredients such as witch hazel, or hydrocortisone and lidocaine, which can temporarily relieve pain and itching.
Hydrocortisone is a steroid that can thin your skin when used for more than a week. Ask your health care provider how long you should use it.
External hemorrhoid thrombectomy
If a painful blood clot has formed within an external hemorrhoid, your health care provider can remove the hemorrhoid. Removal can provide relief right away. This procedure, done with a medicine that numbs a part of the body, also called a local anesthetic, works best when done within 72 hours of getting a clot.
Minimally invasive procedures
For bleeding that doesn't stop or for painful hemorrhoids, your health care provider might recommend one of the other minimally invasive procedures available. These treatments can be done in your provider's office or another outpatient setting. They don't usually require numbing medicine.
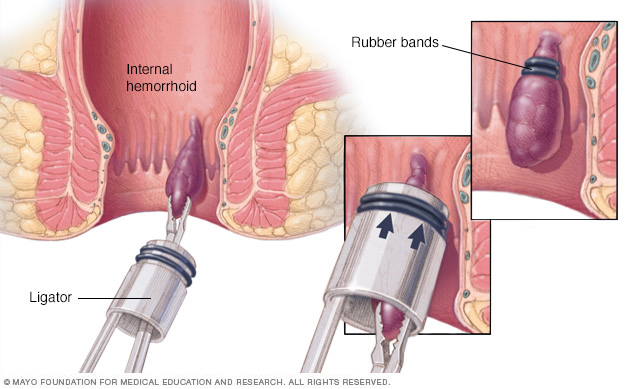
-
Rubber band ligation. Your health care provider places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its blood flow. The hemorrhoid withers and falls off within a week.
Hemorrhoid banding can be uncomfortable and cause bleeding. The bleeding might begin 2 to 4 days after the procedure but is rarely severe. Sometimes, more-serious complications can occur.
- Sclerotherapy. With sclerotherapy, your health care provider injects a chemical solution into the hemorrhoid tissue to shrink it. While the injection causes little or no pain, it might be less effective than rubber band ligation.
- Coagulation. Coagulation techniques use laser or infrared light or heat. They cause small, bleeding internal hemorrhoids to harden and shrivel. Coagulation has few side effects and usually causes little discomfort.
Surgical procedures
Only a small percentage of people with hemorrhoids need surgery to remove them. However, if other procedures haven't worked or you have large hemorrhoids, your health care provider might recommend one of the following:
-
Hemorrhoid removal, also called a hemorrhoidectomy. Your surgeon removes extra tissue that causes bleeding by using one of various techniques. The surgery can be done with a local anesthetic combined with a medicine to help you feel calm or less anxious, also called a sedative. Spinal anesthesia or general anesthesia also may be used.
Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications can include temporarily having a hard time urinating, which can lead to urinary tract infections. This complication happens mainly after spinal anesthesia.
Most people have some pain after the procedure, which medicines can relieve. Soaking in a warm bath also might help.
-
Hemorrhoid stapling. This procedure, called stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. It is typically used only for internal hemorrhoids.
Stapling generally involves less pain than hemorrhoidectomy and lets you get back to regular activities sooner. Compared with hemorrhoidectomy, however, stapling has been associated with a greater risk of hemorrhoids coming back and rectal prolapse. Rectal prolapse is when part of the rectum pushes through the anus.
Complications also can include bleeding, troubles emptying the bladder and pain. A rare complication is a life-threatening blood infection called sepsis.
Talk with your health care provider about the best option for you.
Preparing for an appointment
If you have symptoms of hemorrhoids, make an appointment with your primary care provider. If needed, your provider might refer you to one or more specialists for evaluation and treatment. These may include a doctor with expertise in the digestive system, called a gastroenterologist, or a colon and rectal surgeon.
Here are some suggestions to help you get ready for your appointment.
What you can do
Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance.
Make a list of:
- Your symptoms and how long you've noticed them.
- Key personal information, including typical bowel habits and diet, especially your fiber intake.
- All medicines, vitamins or supplements you take, including doses.
- Questions to ask your health care provider.
For hemorrhoids, some questions to ask your provider include:
- What's the likely cause of my symptoms?
- Is my condition likely to be temporary or permanent?
- Am I at risk of complications related to this condition?
- What treatment approach do you recommend?
- If treatments we try first don't work, what will you recommend next?
- Am I a candidate for surgery? Why or why not?
- Are there additional self-care steps that might help?
- I have other medical problems. How can I manage these along with hemorrhoids?
Don't hesitate to ask other questions.
What to expect from your doctor
Your health care provider is likely to ask you questions, including:
- How uncomfortable are your symptoms?
- What are your typical bowel habits?
- How much fiber does your diet contain?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Has anyone in your family had hemorrhoids or cancer of the colon, rectum or anus?
- Have you had a change in your bowel habits?
- During bowel movements, have you noticed blood on your toilet paper, dripping into the toilet or mixed into your stools?
What you can do in the meantime
Before your appointment, take steps to soften your stools. Eat more high-fiber foods, such as fruits, vegetables and whole grains. Consider a nonprescription fiber supplement, such as Metamucil or Citrucel. Drinking 6 to 8 glasses of water a day also might help relieve your symptoms.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


