Overview
Heart disease describes a range of conditions that affect the heart. Heart disease includes:
- Blood vessel disease, such as coronary artery disease.
- Irregular heartbeats, called arrhythmias.
- Heart conditions that you're born with, called congenital heart defects.
- Disease of the heart muscle.
- Heart valve disease.
Many forms of heart disease can be prevented or treated with healthy lifestyle choices.
Symptoms
Heart disease symptoms depend on the type of heart disease.
Symptoms of heart disease in the blood vessels
Coronary artery disease is a common heart condition that affects the major blood vessels that supply the heart muscle. A buildup of fats, cholesterol and other substances in and on the artery walls usually causes coronary artery disease. This buildup is called plaque. The buildup of plaque in the arteries is called atherosclerosis (ath-ur-o-skluh-ROE-sis). Atherosclerosis reduces blood flow to the heart and other parts of the body. It can lead to a heart attack, chest pain or a stroke.
Symptoms of coronary artery disease can include:
- Chest pain, chest tightness, chest pressure and chest discomfort, called angina.
- Shortness of breath.
- Pain in the neck, jaw, throat, upper belly or back.
- Pain, numbness, weakness or coldness in the legs or arms if the blood vessels in those body areas are narrowed.
You might not be diagnosed with coronary artery disease until you have a heart attack, angina, a stroke or heart failure. It's important to watch for heart symptoms. Talk with your healthcare team about any concerns. Heart disease can sometimes be found early with regular health checkups.
Heart disease symptoms caused by irregular heartbeats, called arrhythmias
The heart may beat too quickly, too slowly or irregularly. Heart arrhythmia symptoms can include:
- Chest pain or discomfort.
- Dizziness.
- Fainting or almost fainting.
- Fluttering in the chest.
- Lightheadedness.
- Racing heartbeat.
- Shortness of breath.
- Slow heartbeat.
Heart disease symptoms caused by congenital heart defects
A congenital heart defect is a heart condition present at birth. Serious congenital heart defects usually are noticed soon after birth. Congenital heart defect symptoms in children could include:
- Blue or gray skin. Depending on skin color, these changes may be easier or harder to see.
- Swelling in the legs, belly area or areas around the eyes.
- In an infant, shortness of breath during feedings, leading to poor weight gain.
Some congenital heart defects may not be found until later in childhood or during adulthood. Symptoms may include:
- Getting very short of breath during exercise or activity.
- Easily tiring during exercise or activity.
- Swelling of the hands, ankles or feet.
Heart disease symptoms caused by diseased heart muscle, called cardiomyopathy
In the beginning, cardiomyopathy may not cause noticeable symptoms. As the condition gets worse, symptoms may include:
- Dizziness, lightheadedness and fainting.
- Fatigue.
- Feeling short of breath during activity or at rest.
- Feeling short of breath at night when trying to sleep, or waking up short of breath.
- Rapid, pounding or fluttering heartbeats.
- Swollen legs, ankles or feet.
Heart disease symptoms caused by heart valve disease
The heart has four valves. The valves open and close to move blood through the heart. Many things can damage the heart valves. If a heart valve is narrowed, it's called stenosis. If a heart valve lets blood flow backward, it's called regurgitation.
Symptoms of heart valve disease depend on which valve isn't working right. Symptoms may include:
- Chest pain.
- Fainting or almost fainting.
- Fatigue.
- Irregular heartbeats.
- Shortness of breath.
- Swollen feet or ankles.
When to see a doctor
Get emergency medical help if you have these heart disease symptoms:
- Chest pain.
- Shortness of breath.
- Fainting.
Always call 911 or your local emergency number if you think you might be having a heart attack.
If you think you may have symptoms of heart disease, make an appointment for a health checkup.
Heart disease is easier to treat when found early.
Causes
Heart disease causes depend on the specific type of heart disease. There are many different types of heart disease.
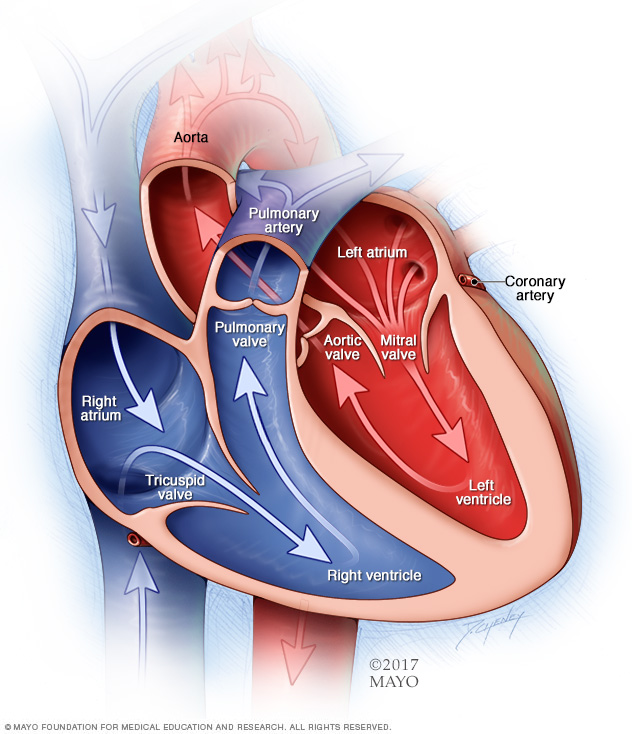
How the heart works
To understand the causes of heart disease, it may help to understand how the heart works.
- The heart has four chambers. The two upper chambers are called the atria. The two lower chambers are called the ventricles.
- The right side of the heart moves blood to the lungs through blood vessels called the pulmonary arteries.
- In the lungs, blood gets oxygen. The oxygen-rich blood goes to the left side of the heart through the pulmonary veins.
- The left side of the heart then pumps the blood through the body's main artery, called the aorta. The blood then goes to the rest of the body.
Heart valves
Four valves in the heart keep blood flowing in the right direction. These valves are:
- Aortic valve.
- Mitral valve.
- Pulmonary valve.
- Tricuspid valve.
Each valve has flaps, called leaflets or cusps. The flaps open and close once during each heartbeat. If a valve flap doesn't open or close properly, less blood moves out of the heart to the rest of the body.
Heartbeats
The heart's electrical system keeps the heart beating. The heart's electrical signals start in a group of cells at the top of the heart called the sinus node. They pass through a pathway between the upper and lower heart chambers called the atrioventricular (AV) node. The movement of the signals causes the heart to squeeze and pump blood.
Causes of coronary artery disease
A buildup of fatty substances in the arteries, called atherosclerosis, is the most common cause of coronary artery disease. Risk factors include an unhealthy diet, lack of exercise, obesity, and smoking. Healthy-lifestyle choices can help lower the risk of atherosclerosis.
Causes of irregular heartbeats, called arrhythmias
Common causes of arrhythmias or conditions that can lead to them include:
- Heart muscle disease, called cardiomyopathy.
- Coronary artery disease.
- Diabetes.
- Illegal drugs such as cocaine.
- Emotional stress.
- Too much alcohol or caffeine.
- Heart conditions present at birth, called congenital heart defects.
- High blood pressure.
- Smoking.
- Heart valve disease.
- Some medicines, herbs and supplements.
Causes of congenital heart defects
A congenital heart defect happens while a baby is growing in the womb. Healthcare professionals aren't sure exactly what causes most congenital heart defects. But gene changes, some medical conditions, some medicines, and environmental or lifestyle factors may play a role.
Causes of heart muscle disease, called cardiomyopathy
The cause of cardiomyopathy depends on the type. There are three types:
- Dilated cardiomyopathy. This is the most common type of cardiomyopathy. The cause is often unknown. It may be passed down through families, which means it's inherited.
- Hypertrophic cardiomyopathy. This type is usually passed down through families.
- Restrictive cardiomyopathy. This type of cardiomyopathy can happen for no known reason. Sometimes a buildup of protein called amyloid causes it. Other causes include connective tissue disorders.
Causes of heart valve disease
Many things can cause a damaged or diseased heart valve. Some people are born with heart valve disease. If this happens, it's called congenital heart valve disease.
Other causes of heart valve disease can include:
- Rheumatic fever.
- Infection in the lining of the heart valves, called infectious endocarditis.
- Connective tissue disorders.
Risk factors
Risk factors for heart disease include:
- Age. Growing older increases the risk of damaged and narrowed arteries and a weakened or thickened heart muscle.
- Sex assigned at birth. Men are generally at greater risk of heart disease. The risk in women increases after menopause.
- Family history. A family history of heart disease increases the risk of coronary artery disease, especially if a parent developed it at an early age. That means before age 55 for a male relative, such as a brother or your father, and 65 for a female relative, such as your mother or a sister.
- Smoking. If you smoke, quit. Substances in tobacco smoke damage the arteries. Heart attacks are more common in people who smoke than in people who don't smoke. Talk with a healthcare professional if you need help quitting.
- Unhealthy diet. Diets high in fat, salt, sugar and cholesterol have been linked to heart disease.
- High blood pressure. High blood pressure that's not controlled can cause the arteries to become hard and thick. These changes alter blood flow to the heart and body.
- High cholesterol. Having high cholesterol increases the risk of atherosclerosis. Atherosclerosis has been linked to heart attack and stroke.
- Diabetes. Diabetes increases the risk of heart disease. Obesity and high blood pressure increase the risk of diabetes and heart disease.
- Obesity. Excess weight typically worsens other heart disease risk factors.
- Lack of exercise. Being inactive is associated with many forms of heart disease and some of its risk factors too.
- Stress. Emotional stress may damage the arteries and make other heart disease risk factors worse.
- Poor dental health. Having unhealthy teeth and gums makes it easier for germs to get into the bloodstream and travel to the heart. This can cause an infection called endocarditis. Brush and floss your teeth often. Also get regular dental checkups.
Complications
Possible complications of heart disease are:
- Heart failure. This is one of the most common complications of heart disease. The heart can't pump enough blood to meet the body's needs.
- Heart attack. A heart attack can happen if a piece of plaque in an artery or a blood clot moves to the heart.
- Stroke. The risk factors that lead to heart disease also can lead to an ischemic stroke. This type of stroke happens when the arteries to the brain are narrowed or blocked. Too little blood reaches the brain.
- Aneurysm. An aneurysm is a bulge in the wall of an artery. If an aneurysm bursts, you may have life-threatening internal bleeding.
- Peripheral artery disease. In this condition, the arms or legs — usually the legs — don't get enough blood. This causes symptoms, most notably leg pain when walking, called claudication. Atherosclerosis can lead to peripheral artery disease.
- Sudden cardiac arrest. Sudden cardiac arrest is the sudden loss of heart activity, breathing and consciousness. It's usually due to a problem with the heart's electrical system. Sudden cardiac arrest is a medical emergency. If not treated immediately, it results in sudden cardiac death.
Prevention
The same lifestyle changes used to manage heart disease also may help prevent it. Try these heart-healthy tips:
- Don't smoke.
- Eat a diet that's low in salt and saturated fat.
- Exercise at least 30 minutes a day on most days of the week.
- Maintain a healthy weight.
- Reduce and manage stress.
- Control high blood pressure, high cholesterol and diabetes.
- Get good sleep. Adults should aim for 7 to 9 hours daily.
Diagnosis
To diagnose heart disease, a healthcare professional examines you and listens to your heart. You are usually asked questions about your symptoms and your personal and family medical history.
Tests
Many different tests are used to diagnose heart disease.
- Blood tests. Certain heart proteins slowly leak into the blood after heart damage from a heart attack. Blood tests can be done to check for these proteins. A high-sensitivity C-reactive protein (CRP) test checks for a protein linked to inflammation of the arteries. Other blood tests may be done to check cholesterol and blood sugar levels.
- Chest X-ray. A chest X-ray shows the condition of the lungs. It can show if the heart is enlarged.
- Electrocardiogram (ECG or EKG). An ECG is a quick and painless test that records the electrical signals in the heart. It can tell if the heart is beating too fast or too slow.
- Holter monitoring. A Holter monitor is a portable ECG device that's worn for a day or more to record the heart's activity during daily activities. This test can detect irregular heartbeats that aren't found during a regular ECG exam.
- Echocardiogram. This noninvasive exam uses sound waves to create detailed images of the heart in motion. It shows how blood moves through the heart and heart valves. An echocardiogram can help determine if a valve is narrowed or leaking.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is checked. Exercise tests help reveal how the heart responds to physical activity and whether heart disease symptoms occur during exercise. If you can't exercise, you might be given medicine that affects the heart like exercise does.
- Cardiac catheterization. This test can show blockages in the heart arteries. A long, thin flexible tube called a catheter is inserted in a blood vessel, usually in the groin or wrist, and guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images taken during the test.
- Heart CT scan, also called cardiac CT scan. In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest.
- Heart magnetic resonance imaging (MRI) scan. A cardiac MRI uses a magnetic field and computer-generated radio waves to create detailed images of the heart.
Treatment
Heart disease treatment depends on the cause and type of heart damage. Treatment for heart disease may include:
- Lifestyle changes such as eating a diet low in salt and saturated fat, getting more exercise, and not smoking.
- Medicines.
- A heart procedure.
- Heart surgery.
Medications
You may need medicines to control heart disease symptoms and prevent complications. The type of medicine used depends on the type of heart disease.
Surgery or other procedures
Some people with heart disease may need a heart procedure or surgery. The type of treatment depends on the type of heart disease and how much damage has happened to the heart.
Lifestyle and home remedies
Lifestyle changes are an important part of heart disease treatment and prevention. The following changes are recommended to improve heart health:
- Don't smoke. Smoking is a major risk factor for heart disease. If you smoke and can't quit, talk with your healthcare team about programs or treatments that can help.
- Eat healthy foods. Eat plenty of fruits, vegetables and whole grains. Limit sugar, salt and saturated fats.
- Control blood pressure. Uncontrolled high blood pressure increases the risk of serious health conditions. Get your blood pressure checked at least every two years if you're 18 or older. If you have risk factors for heart disease or are over age 40, you may need more-frequent checks. Ask your healthcare professional what blood pressure reading is best for you.
- Get a cholesterol test. Get a cholesterol test when you're in your 20s and then at least every 4 to 6 years. You may need to start testing earlier if high cholesterol is in your family history. You may need cholesterol checks more often if your test results aren't in a desirable range or you have risk factors for heart disease.
- Manage diabetes. If you have diabetes, controlling your blood sugar can help reduce the risk of heart disease.
- Exercise. Staying active keeps the heart healthy. Exercise at least 30 minutes a day on most days of the week. Talk with your healthcare team about the amount and type of exercise that's best for you.
- Keep a healthy weight. Being overweight increases the risk of heart disease. Ask your healthcare professional what weight is best for you.
- Manage stress. Find ways to help reduce emotional stress. Some tips are to get more exercise, practice mindfulness and connect with others in support groups.
- Practice good hygiene. Regularly wash your hands and brush and floss your teeth to keep yourself healthy.
- Get good sleep. Poor sleep may increase the risk of heart disease and other long-term health conditions. Adults should try to get 7 to 9 hours of sleep daily. Kids often need more. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk with your healthcare professional about strategies that might help.
Coping and support
Here are some ways to help manage heart disease and improve quality of life:
- Cardiac rehabilitation. This is a personalized program of education and exercise. It includes exercise training, emotional support and education about a heart-healthy lifestyle. The supervised program is often recommended after a heart attack or heart surgery.
- Support groups. Connecting with friends and family or joining a support group is a good way to reduce stress. You may find that talking about your concerns with others in similar situations can help.
- Get regular health checkups. Seeing your healthcare professional regularly helps make sure you're properly managing your heart disease.
Preparing for an appointment
Some types of heart disease are found at birth or during an emergency, for example, when someone has a heart attack. You may not have time to prepare.
If you think you have heart disease or are at risk of heart disease because of family history, see your healthcare professional. You may be referred to a doctor trained in heart diseases. This type of doctor is called a cardiologist.
Here's some information to help you prepare for your appointment.
What you can do
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet. For example, you may be told not to eat or drink for a few hours before a cholesterol test.
- Write down symptoms you're having, including any that seem unrelated to heart disease.
- Write down important personal information. Note if you have a family history of heart disease, stroke, high blood pressure or diabetes. Also write down any major stresses or recent life changes.
- Make a list of medicines, vitamins or supplements you're taking. Include the dosages.
- Take someone along, if possible. Someone who goes with you can help you remember information you're given.
- Be prepared to talk about your diet and any smoking and exercise habits. If you don't already follow a diet or exercise routine, ask your healthcare team how to get started.
- Write down questions to ask your healthcare professional.
For heart disease, some basic questions to ask your healthcare professional include:
- What is the likely cause of my symptoms or condition?
- What are other possible causes?
- What tests do I need?
- What's the best treatment?
- What are the options to the treatment that you're suggesting?
- What foods should I eat or avoid?
- What's an appropriate level of physical activity?
- How often should I be screened for heart disease? For example, how often do I need a cholesterol test?
- I have other health conditions. How do I manage them together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Are there brochures or other materials that I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your healthcare team is likely to ask you many questions, such as:
- When did your symptoms begin?
- Do you always have symptoms or do they come and go?
- On a scale of 1 to 10 with 10 being the worst, how bad are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, makes your symptoms worse?
- Do you have a family history of heart disease, diabetes, high blood pressure or other serious illness?
What you can do in the meantime
It's never too early to make healthy-lifestyle changes. Eat a healthy diet, get more exercise and don't smoke. A healthy lifestyle is the best protection against heart disease and its complications.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


