Overview
Genital warts are one of the most common types of sexually transmitted infections. The virus that causes the warts is called human papillomavirus (HPV). There are various types of HPV. And nearly all sexually active people will become infected with at least one type at some point.
Genital warts affect the moist tissues of the genital area. They can look like small, skin-colored bumps. The bumps may resemble cauliflower. Often, the warts are too small to be seen with your eyes.
Some strains of genital HPV can cause genital warts. Others can cause cancer. Vaccines can help protect against certain strains of genital HPV.
Symptoms
Genital warts can grow on the:
- Vulva.
- Walls of the vagina.
- Area between the outer part of the genitals and the anus.
- Anal canal.
- Cervix.
- Tip or shaft of the penis.
- Scrotum.
- Anus.
Genital warts also can form in the mouth or throat of a person who has had oral sex with an infected person.
The symptoms of genital warts include:
- Small swellings in the genital area that may be skin-colored or a different color.
- A cauliflower-like shape caused by a few warts close together.
- Itching or discomfort in your genital area.
- Bleeding with sex.
Genital warts can be so small and flat that you can't see them. But rarely, they can multiply into large clusters in someone with a weakened immune system.
When to see a doctor
See a health care professional if you or your partner gets bumps or warts in the genital area.

Causes
The human papillomavirus (HPV) causes warts. There are more than 40 strains of HPV that affect the genital area.
Genital warts almost always are spread through sexual contact. Even if your warts are too small to be seen, you could spread the infection to your sexual partner.
Risk factors
Most people who are sexually active get infected with genital HPV at some time. Factors that can raise your risk of infection include:
- Not getting the HPV vaccine.
- Having sex without a condom or with more than one partner.
- Having had another sexually transmitted infection.
- Having sex with a partner whose sexual history you don't know.
- Becoming sexually active at a young age.
- Having a weakened immune system, such as from HIV or medicines from an organ transplant.
Complications
An HPV infection can lead to health problems such as:
-
Cancer. Cervical cancer has been closely linked with genital HPV infection. Certain types of HPV also are linked with cancers of the vulva, anus, penis, and mouth and throat.
HPV infection doesn't always lead to cancer. But it's important for women to have regular Pap tests, which check for cancer of the cervix. Pap tests are key for those who've been infected with higher-risk types of HPV.
-
Problems during pregnancy. Rarely during pregnancy, warts can become larger. This makes it hard to urinate. Warts on the vaginal wall can hinder the stretching of vaginal tissues during childbirth. Large warts on the vulva or in the vagina can bleed when stretched during delivery.
Very rarely, a baby born to a pregnant person with genital warts get warts in the throat. The baby might need surgery to keep the airway from being blocked.
Prevention
Get the HPV vaccine to help prevent genital warts. And if you have sex, limit your number of partners. It's safest to have sex with just one partner who only has sex with you. It's also a good idea to use a condom every time you have sex. But this won't fully protect you from genital warts. That's because HPV can infect parts of the body that the condom doesn't cover.
Vaccination
In the United States, the Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination for girls and boys ages 11 and 12. But the vaccine can be given as early as age 9.
It's ideal for children to receive the vaccine before they have sexual contact.
Most often, side effects from the vaccines are mild. They include soreness where the shot was given, headaches, a low-grade fever or flu-like symptoms.
The CDC now recommends that all 11- and 12-year-olds receive two doses of HPV vaccine 6 to 12 months apart. The agency used to recommend a three-dose schedule. Younger children ages 9 and 10 and teens ages 13 and 14 also can get two doses of the vaccine. Research has shown that two doses work for children under 15.
Teens and young adults who start the vaccine series later, at ages 15 through 26, should receive three doses. The CDC recommends that the second dose be given 1 to 2 months after the first. The third dose should be given 6 months after the first.
The CDC now recommends catch-up HPV vaccinations for all people through age 26 who aren't fully vaccinated.
The U.S. Food and Drug Administration approved the use of the Gardasil 9 HPV vaccine for males and females ages 9 to 45. If you're ages 27 to 45, ask your health care team about your risks to decide if you should get the HPV vaccine.
Other HPV vaccines are offered outside of the United States. Talk with your health care team about when to get vaccinated and how many doses are needed.
Diagnosis
Health care professionals often can find genital warts during a physical exam. Sometimes, a small piece of tissue needs to be removed and checked by a lab. This is called a biopsy.
Pap tests
For women, it's important to have regular Pap tests. These tests can help find changes in the vagina and cervix caused by genital warts. They also can find the early signs of cervical cancer.
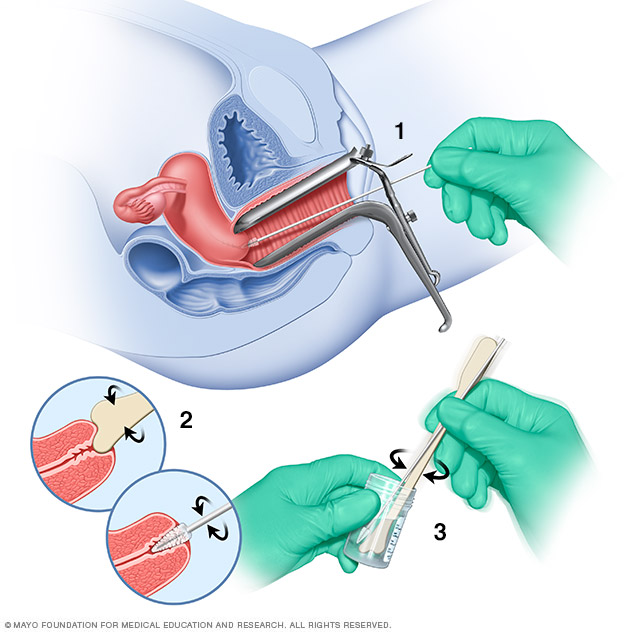
During a Pap test, a device called a speculum holds open the vagina. Then, the health care professional can see the passage between the vagina and uterus, called the cervix. A long-handled tool collects a small sample of cells from the cervix. The cells are checked with a microscope for irregular changes.
HPV test
Only a few types of genital HPV have been linked to cervical cancer. A sample of cervical cells, taken during a Pap test, can be tested for these cancer-causing HPV strains.
Most often, this test is done for women age 30 and older. It isn't as useful for younger women. That's because for them, HPV usually goes away without treatment.
Treatment
If your warts don't cause discomfort, you might not need treatment. But medicine or surgery can help you clear an outbreak if you have itching, burning and pain. Treatment also can help if you're concerned about spreading the infection.
Warts often return after treatment though. And there is no treatment for the virus itself.
Medications
Genital wart treatments that can go on the skin include:
-
Imiquimod (Zyclara). This cream seems to boost the immune system's ability to fight genital warts. Do not have sexual contact while the cream is on your skin. It might weaken condoms and diaphragms and irritate your partner's skin.
One possible side effect is a change in skin color where the medicine is used. Other side effects might include blisters, body aches or pain, a cough, rashes, and fatigue.
-
Podophyllin (Podocon-25) and podofilox (Condylox). Podophyllin is a plant-based substance that destroys genital wart tissue. A health care professional puts this solution on your skin. Podofilox contains the same active compound, but you can put it on at home.
Never place podofilox inside your body. Also, this medicine isn't recommended for use during pregnancy. Side effects can include mild skin irritation, sores and pain.
- Trichloroacetic acid. This chemical treatment burns off genital warts. It also can treat warts inside the body. Side effects can include mild skin irritation, sores and pain.
- Sinecatechins (Veregen). This ointment can treat genital warts on the body and warts in or around the anus. Side effects can include a change in skin color, itching or burning, and pain.
Do not try to treat genital warts with wart removers sold in stores. These medicines aren't meant for use in the genital area.
Surgery
You might need surgery to remove larger warts or ones that don't get better with medicine. If you're pregnant, you may need surgery to remove warts that your baby could come in contact with during delivery. Surgeries for genital warts include:
- Freezing with liquid nitrogen. This also is called cryotherapy. Freezing works by causing a blister to form around the wart. As the skin heals, the warts slough off and new skin appears. You might need to repeat the treatment. The main side effects include pain and swelling.
- Electrocautery. This procedure uses an electric current to burn off warts. You might have some pain and swelling afterward.
- Surgical excision. Warts can be cut off during surgery. You'll need medicine called anesthesia that keeps you from feeling pain during this treatment. You might have pain afterward.
- Laser treatments. This approach uses an intense beam of light. It can be expensive. Most often, it's saved for warts that are extensive and tough to treat. Side effects can include scarring and pain.
Preparing for an appointment
You'll likely start by seeing your health care professional.
What you can do
Make a list of your:
- Symptoms and when they began. Describe your symptoms. If you have a sexual partner, note whether your partner has had similar symptoms.
- Sexual history. Include any situations that might have exposed you to infections. This is key if you've had sex without a condom or sex with a new partner.
- Key medical information. Include other conditions you're being treated for.
- All medicines, vitamins or other supplements you take. Include the doses.
For genital warts, some basic questions to ask your health care professional include:
- What tests do I need?
- Should I also be tested for other sexually transmitted infections?
- What treatment do you recommend, if any?
- How soon after I start treatment can I expect to get better?
- Am I contagious? How can I lower the risk of passing this infection to others?
- Should my partner be tested for this condition?
- When can I safely have sex again?
- Will my genital warts come back?
- Am I at risk of health problems related to genital warts?
- How often should I be screened for other health conditions related to genital warts?
- Are there printed materials I can have? What websites do you recommend?
Feel free to ask other questions.
What to expect from your doctor
Your health care professional is likely to ask you questions, including:
- How severe are your symptoms?
- Do you practice safe sex? Have you always done so?
- Have you recently had sex with a new partner?
- Has your partner been tested for sexually transmitted infections?
- Have you had the HPV vaccine? When?
- Are you pregnant or planning to become pregnant?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


