Overview
Gastritis is a general term for a group of conditions with one thing in common: Inflammation of the lining of the stomach. The inflammation of gastritis is most often the result of infection with the same bacterium that causes most stomach ulcers or the regular use of certain pain relievers. Drinking too much alcohol also can contribute to gastritis.
Gastritis may occur suddenly (acute gastritis) or appear slowly over time (chronic gastritis). In some cases, gastritis can lead to ulcers and an increased risk of stomach cancer. For most people, however, gastritis isn't serious and improves quickly with treatment.
Symptoms
Gastritis doesn't always cause symptoms. When it does, the symptoms of gastritis may include:
- Gnawing or burning ache or pain, called indigestion, in your upper belly. This feeling may become either worse or better after eating.
- Nausea.
- Vomiting.
- A feeling of fullness in your upper abdomen after eating.
When to see a doctor
Nearly everyone has had indigestion and stomach irritation at some point. Usually, indigestion doesn't last long and doesn't require medical care. See your healthcare professional if you have symptoms of gastritis for a week or longer.
Seek medical attention right away if you have severe pain or if you have vomiting where you cannot hold any food down. Also seek attention right away if you feel lightheaded or dizzy. Tell your healthcare professional if your stomach discomfort happens after taking medicines, especially aspirin or other pain relievers.
If you are vomiting blood, have blood in your stools or have stools that appear black, see your healthcare professional right away to find the cause.
Causes
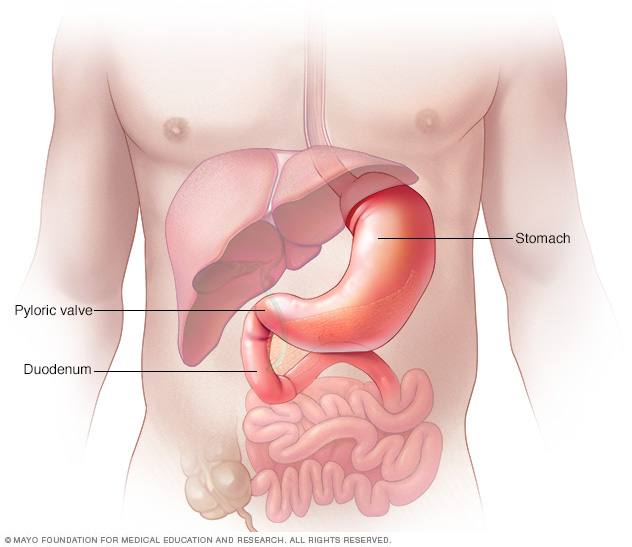
Gastritis is an inflammation of the stomach lining. The stomach lining is a mucus-lined barrier that protects the stomach wall. Weaknesses or injury to the barrier allows digestive juices to damage and inflame the stomach lining. Several diseases and conditions can increase the risk of gastritis. These include inflammatory conditions, such as Crohn's disease.
Risk factors
Factors that increase your risk of gastritis include:
- Bacterial infection. A bacterial infection called Helicobacter pylori, also known as H. pylori, is one of the most common worldwide human infections. However, only some people with the infection develop gastritis or other upper gastrointestinal disorders. Healthcare professionals believe sensitivity to the germs could be inherited. Sensitivity also may be caused by lifestyle choices, such as smoking and diet.
- Regular use of pain relievers. Pain relievers known as nonsteroidal anti-inflammatory drugs, also called NSAIDs, can cause both acute gastritis and chronic gastritis. NSAIDs include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve, Anaprox DS). Using these pain relievers regularly or taking too much of these medicines may damage the stomach lining.
- Older age. Older adults have an increased risk of gastritis because the stomach lining tends to thin with age. Older adults also have an increased risk because they are more likely to have H. pylori infection or autoimmune disorders than younger people are.
- Excessive alcohol use. Alcohol can irritate and break down your stomach lining. This makes your stomach more vulnerable to digestive juices. Excessive alcohol use is more likely to cause acute gastritis.
- Stress. Severe stress due to major surgery, injury, burns or severe infections can cause acute gastritis.
- Cancer treatment. Chemotherapy medicines or radiation treatment can increase your risk of gastritis.
-
Your own body attacking cells in your stomach. Called autoimmune gastritis, this type of gastritis occurs when your body attacks the cells that make up your stomach lining. This reaction can wear away at your stomach's protective barrier.
Autoimmune gastritis is more common in people with other autoimmune disorders. These include Hashimoto's disease and type 1 diabetes. Autoimmune gastritis also can be associated with vitamin B-12 deficiency.
- Other diseases and conditions. Gastritis may be associated with other medical conditions. These may include HIV/AIDS, Crohn's disease, celiac disease, sarcoidosis and parasitic infections.
Complications
Left untreated, gastritis may lead to stomach ulcers and stomach bleeding. Rarely, some forms of chronic gastritis may increase your risk of stomach cancer. This risk is increased if you have extensive thinning of the stomach lining and changes in the lining's cells.
Tell your healthcare professional if your symptoms aren't improving despite treatment for gastritis.
Diagnosis
Your healthcare professional is likely to suspect gastritis after talking to you about your medical history and performing an exam. However, you also may have one or more of the following tests to find the exact cause.
-
Tests for H. pylori. Your healthcare professional may recommend tests such as a stool test or breath test to determine whether you have H. pylori. Which type of test you have depends on your situation.
For the breath test, you drink a small glass of clear, tasteless liquid that contains radioactive carbon. H. pylori germs break down the test liquid in your stomach. Later, you blow into a bag, which is then sealed. If you're infected with H. pylori, your breath sample will contain the radioactive carbon.
-
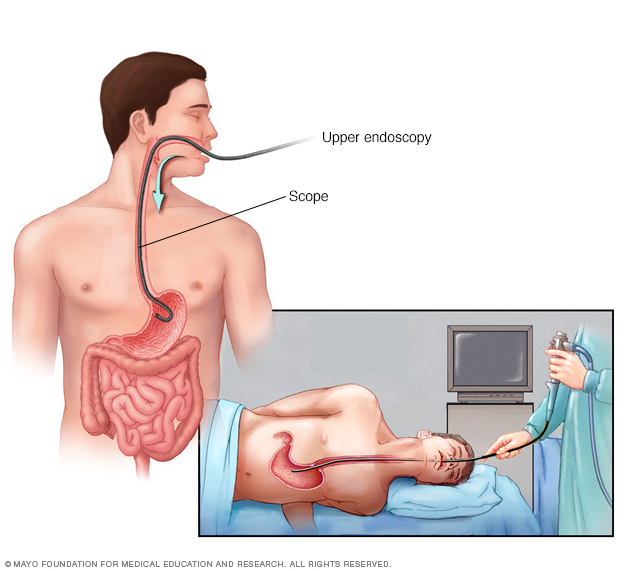
Passing a thin, flexible scope down the throat, called an endoscopy. Endoscopy is a procedure to examine the digestive system with a long, thin tube with a tiny camera, called an endoscope. The endoscope passes down the throat, into the esophagus, stomach and small intestine. Using the endoscope, your healthcare professional looks for signs of inflammation. Depending on your age and medical history, your healthcare professional may recommend this as a first test instead of testing for H. pylori.
If a suspicious area is found, your healthcare professional may remove small tissue samples, called a biopsy, to test in a lab. A biopsy also can identify the presence of H. pylori in your stomach lining.
- X-ray of your upper digestive system. X-rays can create images of your esophagus, stomach and small intestine to look for anything unusual. You may have to swallow a white, metallic liquid that contains barium. The liquid coats your digestive tract and makes an ulcer more visible. This procedure is called a barium swallow.
Treatment
Treatment of gastritis depends on the specific cause. Acute gastritis caused by NSAIDs or alcohol may be relieved by stopping use of those substances.
Medicines used to treat gastritis include:
- Antibiotics to kill H. pylori. For H. pylori in your digestive tract, your healthcare professional may recommend a combination of antibiotics to kill the germs. Be sure to take the full antibiotic prescription, usually for 7 to 14 days. You also may take a medicine to block acid production. Once treated, your healthcare professional will retest you for H. pylori to be sure it has been destroyed.
-
Medicines that block acid production and promote healing. Medicines called proton pump inhibitors help reduce acid. They do this by blocking the action of the parts of cells that produce acid. You may get a prescription for proton pump inhibitors, or you can buy them without a prescription.
Long-term use of proton pump inhibitors, particularly at high doses, may increase your risk of hip, wrist and spine fractures. Ask your healthcare professional whether a calcium supplement may reduce this risk.
- Medicines to reduce acid production. Acid blockers, also called histamine blockers, reduce the amount of acid released into your digestive tract. Reducing acid relieves gastritis pain and encourages healing. You may get a prescription for an acid blocker, or you can buy one without a prescription.
- Medicines that neutralize stomach acid. Your healthcare professional may include an antacid in your treatment. Antacids neutralize existing stomach acid and can provide rapid pain relief. These help with immediate symptom relief but are generally not used as a primary treatment. Side effects of antacids can include constipation or diarrhea, depending on the main ingredients. Proton pump inhibitors and acid blockers are more effective and have fewer side effects.
Lifestyle and home remedies
You may find some relief from symptoms if you:
- Don't drink alcohol. Alcohol can irritate the mucous lining of your stomach.
- Consider switching pain relievers. If you use pain relievers that increase your risk of gastritis, ask your healthcare professional whether acetaminophen (Tylenol, others) may be an option for you. This medicine is less likely to stir up your stomach problem.
Preparing for an appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
If your healthcare professional thinks that you might have gastritis, you may be referred to a doctor who specializes in digestive disorders, called a gastroenterologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you're experiencing, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down key personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For gastritis, some basic questions to ask include:
- What is likely causing my symptoms or condition?
- Should I be tested for H. pylori, or do I need an endoscopy?
- Could any of my medicines be causing my condition?
- What are other possible causes for my symptoms or condition?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What is the best course of action?
- What are alternatives to the primary approach you're suggesting?
- I have other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed material I can take? What websites do you recommend?
- What will determine whether I should schedule a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- What are your symptoms?
- How severe are your symptoms? Would you describe your stomach pain as mildly uncomfortable or burning?
- Have your symptoms been continuous or occasional?
- Does anything, such as eating certain foods, seem to worsen your symptoms?
- Does anything, such as eating certain foods or taking antacids, seem to improve your symptoms?
- Do you experience any nausea or vomiting?
- Have you recently lost weight?
- How often do you take pain relievers, such as aspirin, ibuprofen or naproxen sodium?
- How often do you drink alcohol, and how much do you drink?
- How would you rate your stress level?
- Have you noticed any black stools or blood in your stool?
- Have you ever had an ulcer?
What you can do in the meantime
Before your appointment, avoid drinking alcohol and eating foods that seem to irritate your stomach. These foods may include those that are spicy, acidic, fried or fatty. But talk to your healthcare professional before stopping any prescription medicines you're taking.
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


