Overview
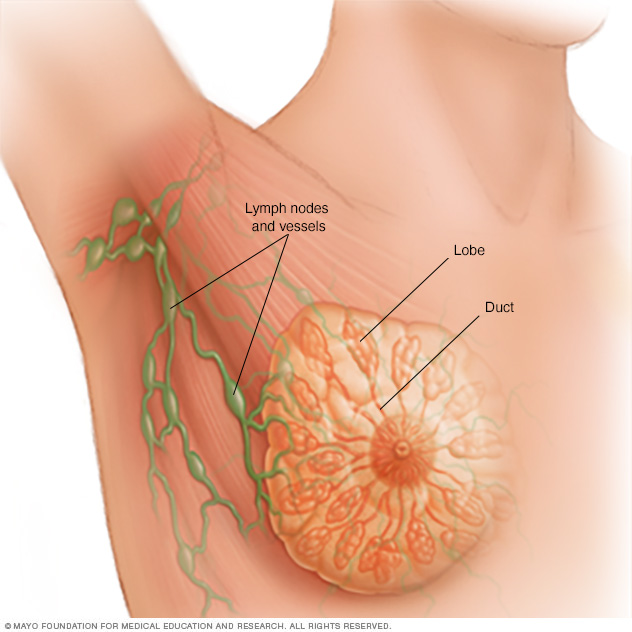
Ductal carcinoma in situ is a very early form of breast cancer. In ductal carcinoma in situ, the cancer cells are confined inside a milk duct in the breast. The cancer cells haven't spread into the breast tissue. Ductal carcinoma in situ is often shortened to DCIS. It's sometimes called noninvasive, preinvasive or stage 0 breast cancer.
DCIS is usually found during a mammogram done as part of breast cancer screening or to investigate a breast lump. DCIS has a low risk of spreading and becoming life-threatening. However, it does require an evaluation and a consideration of treatment options.
Treatment for DCIS often involves surgery. Other treatments may combine surgery with radiation therapy or hormone therapy.
Symptoms
Ductal carcinoma in situ doesn't typically cause symptoms. This early form of breast cancer also is called DCIS.
DCIS can sometimes cause symptoms such as:
- A breast lump.
- Bloody nipple discharge.
DCIS is usually found on a mammogram. It appears as tiny flecks of calcium in the breast tissue. These are calcium deposits, often referred to as calcifications.
When to see a doctor
Make an appointment with your doctor or other healthcare professional if you notice a change in your breasts. Changes to look for may include a lump, an area of puckered or otherwise unusual skin, a thickened region under the skin, and nipple discharge.
Ask your healthcare professional when you should consider breast cancer screening and how often it should be repeated. Most healthcare professionals recommend considering routine breast cancer screening beginning in your 40s.
Causes
It's not clear what causes ductal carcinoma in situ, also called DCIS.
This early form of breast cancer happens when cells inside a breast duct develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
In DCIS, the cancer cells don't yet have the ability to break out of the breast duct and spread into the breast tissue.
Healthcare professionals don't know exactly what causes the changes in the cells that leads to DCIS. Factors that may play a part include lifestyle, environment and DNA changes that run in families.
Risk factors
Several factors may increase the risk of ductal carcinoma in situ, also called DCIS. DCIS is an early form of breast cancer. Risk factors for breast cancer may include:
- A family history of breast cancer. If a parent, sibling or child had breast cancer, your risk of breast cancer is increased. The risk is higher if your family has a history of getting breast cancer at a young age. The risk also is higher if you have multiple family members with breast cancer. Still, most people diagnosed with breast cancer don't have a family history of the disease.
- A personal history of breast cancer. If you've had cancer in one breast, you have an increased risk of getting cancer in the other breast.
- A personal history of breast conditions. Certain breast conditions are a sign of a higher risk of breast cancer. These conditions include lobular carcinoma in situ, also called LCIS, and atypical hyperplasia of the breast. If you've had a breast biopsy that found one of these conditions, you have an increased risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases the risk of breast cancer.
- Beginning menopause at an older age. Beginning menopause after age 55 increases the risk of breast cancer.
- Being female. Women are much more likely than men are to get breast cancer. Everyone is born with some breast tissue, so anyone can get breast cancer.
- Dense breast tissue. Breast tissue is made up of fatty tissue and dense tissue. Dense tissue is made of milk glands, milk ducts and fibrous tissue. If you have dense breasts, you have more dense tissue than fatty tissue in your breasts. Having dense breasts can make it harder to detect breast cancer on a mammogram. If a mammogram showed that you have dense breasts, your risk of breast cancer is increased. Talk with your healthcare team about other tests you might have in addition to mammograms to look for breast cancer.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
- Having your first child at an older age. Giving birth to your first child after age 30 may increase the risk of breast cancer.
- Having never been pregnant. Having been pregnant one or more times lowers the risk of breast cancer. Never having been pregnant increases the risk.
- Increasing age. The risk of breast cancer goes up as you get older.
- Inherited DNA changes that increase cancer risk. Certain DNA changes that increase the risk of breast cancer can be passed from parents to children. The most well-known changes are called BRCA1 and BRCA2. These changes can greatly increase your risk of breast cancer and other cancers, but not everyone with these DNA changes gets cancer.
- Menopausal hormone therapy. Taking certain hormone therapy medicines to control the symptoms of menopause may increase the risk of breast cancer. The risk is linked to hormone therapy medicines that combine estrogen and progesterone. The risk goes down when you stop taking these medicines.
- Obesity. People with obesity have an increased risk of breast cancer.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is higher.
Prevention
Making changes in your daily life may help lower your risk of ductal carcinoma in situ. This early form of breast cancer also is called DCIS. To lower your risk of breast cancer, try to:
Ask about breast cancer screening
Talk with your doctor or other healthcare professional about when to begin breast cancer screening. Ask about the benefits and risks of screening. Together, you can decide what breast cancer screening tests are right for you.
Become familiar with your breasts through breast self-exam for breast awareness
You may choose to become familiar with your breasts by occasionally inspecting them during a breast self-exam for breast awareness. If you find a new change, lumps or other unusual signs in your breasts, tell a healthcare professional right away.
Breast awareness can't prevent breast cancer. But it may help you to better understand the look and feel of your breasts. This might make it more likely that you'll notice if something changes.
Drink alcohol in moderation, if at all
If you choose to drink alcohol, limit the amount you drink to no more than one drink a day. For breast cancer prevention, there is no safe amount of alcohol. So if you're very concerned about your breast cancer risk, you may choose to not drink alcohol.
Exercise most days of the week
Aim for at least 30 minutes of exercise on most days of the week. If you haven't been active lately, ask your healthcare professional whether exercising is OK and start slowly.
Limit hormone therapy during menopause
Combination hormone therapy may increase the risk of breast cancer. Talk with a healthcare professional about the benefits and risks of hormone therapy.
Some people have symptoms during menopause that cause discomfort. These people may decide that the risks of hormone therapy are acceptable to get relief. To reduce the risk of breast cancer, use the lowest dose of hormone therapy possible for the shortest amount of time.
Maintain a healthy weight
If your weight is healthy, work to maintain that weight. If you need to lose weight, ask a healthcare professional about healthy ways to lower your weight. Eat fewer calories and slowly increase the amount you exercise.
Diagnosis
Ductal carcinoma in situ, also called DCIS, is most often discovered during a mammogram used to screen for breast cancer. A mammogram is an X-ray of the breast tissue. If your mammogram shows something concerning, you will likely have additional breast imaging and a biopsy.
Mammogram
If an area of concern was found during a screening mammogram, you may then have a diagnostic mammogram. A diagnostic mammogram takes views at higher magnification from more angles than a mammogram used for screening. This examination evaluates both breasts.
A diagnostic mammogram gives your healthcare team a closer look at any calcium deposits detected in the breast tissue. Calcium deposits, also called calcifications, can sometimes be cancerous.
If the area of concern needs further evaluation, the next step may be an ultrasound and a breast biopsy.
Breast ultrasound
Ultrasound uses sound waves to make images of structures inside the body. A breast ultrasound may give your healthcare team more information about an area of concern. The healthcare team uses this information to decide what tests you might need next.
Removing breast tissue samples for testing
A biopsy is a procedure to remove a sample of tissue for testing in a lab. For DCIS, a healthcare professional removes the sample of breast tissue using a special needle. The needle used is a hollow tube. The healthcare professional puts the needle through the skin on the breast and into the area of concern. The health professional draws out some of the breast tissue. This procedure is called a core needle biopsy.
Often the healthcare professional uses an imaging test to help guide the needle to the right spot. A biopsy that uses ultrasound is called an ultrasound-guided breast biopsy. If it uses X-rays, it's called a stereotactic breast biopsy. The tissue samples are sent to a lab for testing.
In a lab, a doctor who specializes in analyzing blood and body tissue looks at the tissue samples. This doctor is called a pathologist. The pathologist can tell whether cancer cells are present and if so, how aggressive those cells appear to be.

Treatment
Ductal carcinoma in situ can often be cured. Treatment for this very early form of breast cancer often involves surgery to remove the cancer. Ductal carcinoma in situ, also called DCIS, also may be treated with radiation therapy and medicines.
DCIS treatment has a high likelihood of success. In most instances, the cancer is removed and has a low chance of coming back after treatment.
In most people, treatment options for DCIS include:
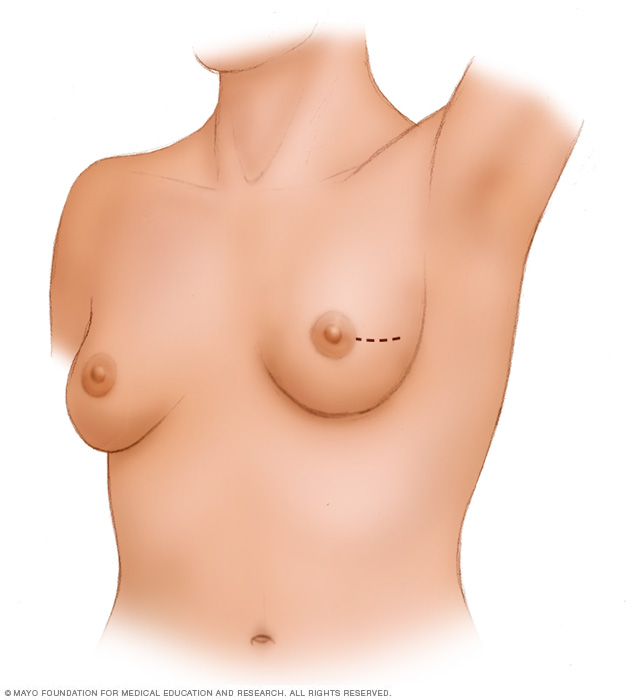
- Breast-conserving surgery, called a lumpectomy, and radiation therapy.
- Breast-removing surgery, called a mastectomy.
In some people, treatment options may include:
- Lumpectomy only.
- Lumpectomy and hormone therapy.
Surgery
If you're diagnosed with DCIS, one of the first decisions you'll have to make is whether to treat the condition with lumpectomy or mastectomy.
-
Lumpectomy. A lumpectomy is surgery to remove the breast cancer and some of the healthy tissue around it. The rest of the breast tissue isn't removed. Other names for this surgery are breast-conserving surgery and wide local excision. Most people who have a lumpectomy also have radiation therapy.
Research suggests that there is a slightly higher risk of the cancer coming back after lumpectomy compared to mastectomy. However, survival rates between the two treatment approaches are very similar.
If you have other serious health conditions, you might consider other options, such as lumpectomy plus hormone therapy, lumpectomy alone or no treatment.
- Mastectomy. A mastectomy is surgery to remove all breast tissue from a breast. Breast reconstruction to restore the appearance of the breast can be done at the same time or in a later procedure, if you desire.
Lumpectomy is a good option for most people with DCIS. But mastectomy may be recommended if:
- You have a large area of DCIS. If the area is large relative to the size of your breast, a lumpectomy may not produce acceptable cosmetic results.
- There's more than one area of DCIS. When there are multiple areas of DCIS, it is called multifocal or multicentric disease. It's difficult to remove multiple areas of DCIS with a lumpectomy. This is especially true if DCIS is found in different parts of the breast.
- Biopsy results show cancer cells at or near the edge of the tissue sample. There may be more DCIS than originally thought. This means that a lumpectomy might not be enough to remove all areas of DCIS. A mastectomy could be needed to remove all of the breast tissue.
- You're not a candidate for radiation therapy. Radiation is usually given after a lumpectomy. Radiation might not be an option if you're in the first trimester of pregnancy or if you've received radiation to your chest or breast in the past. It also might not be recommended if you have a condition that makes you more sensitive to radiation side effects, such as systemic lupus erythematosus.
- You prefer to have a mastectomy. For instance, you might not want a lumpectomy if you don't want to have radiation therapy.
Because DCIS is noninvasive, surgery typically doesn't involve the removal of lymph nodes from under your arm. The chance of finding cancer in the lymph nodes is extremely small.
If your healthcare team thinks the cancer cells may have spread outside the breast duct or if you are having a mastectomy, then some lymph nodes may be removed as part of the surgery.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources.
For DCIS treatment, the radiation is often external beam radiation. During this type of radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body. Less often, the radiation can be placed inside the body. This type of radiation is called brachytherapy.
Radiation therapy is often used after lumpectomy to reduce the chance that DCIS will come back or that it will progress to invasive cancer. But it might not be necessary if you have only a small area of DCIS that is considered slow-growing and was completely removed during surgery.
Hormone therapy
Hormone therapy, also called endocrine therapy, uses medicines to block certain hormones in the body. It's a treatment for breast cancers that are sensitive to the hormones estrogen and progesterone. Healthcare professionals call these cancers estrogen receptor positive and progesterone receptor positive. Cancers that are sensitive to hormones use the hormones as fuel for their growth. Blocking the hormones can cause the cancer cells to shrink or die.
For DCIS, hormone therapy is typically used after surgery or radiation. It lowers the risk that the cancer will come back. It also reduces the risk of developing another breast cancer.
Treatments that can be used in hormone therapy include:
- Medicines that block hormones from attaching to cancer cells. These medicines are called selective estrogen receptor modulators. Examples include tamoxifen and raloxifene (Evista).
- Medicines that stop the body from making estrogen after menopause. These medicines are called aromatase inhibitors. Examples include anastrozole (Arimidex), exemestane (Aromasin) and letrozole (Femara).
Discuss the benefits and risks of hormone therapy with your healthcare team.
Alternative medicine
No alternative medicine treatments have been found to cure ductal carcinoma in situ, also called DCIS. But complementary and alternative medicine therapies may help you cope with side effects of treatment.
Combined with your healthcare team's recommendations, complementary and alternative medicine treatments may provide some comfort. Examples include:
- Art therapy.
- Exercise.
- Meditation.
- Music therapy.
- Relaxation exercises.
- Spirituality.
Coping and support
A diagnosis of ductal carcinoma in situ, also called DCIS, can feel overwhelming. To cope with your diagnosis, it may be helpful to:
Learn enough about DCIS to make decisions about your care
Ask your healthcare team questions about your diagnosis and your pathology results. Use this information to research your treatment options.
Knowing more about your cancer and your options may help you feel more confident when making treatment decisions. Still, some people don't want to know the details of their cancer. If this is how you feel, let your care team know that too.
Find someone to talk with about your feelings
Find a friend or family member who is a good listener. Or talk with a clergy member or counselor. Ask your healthcare team for a referral to a counselor or other professional who works with people who have cancer.
Keep your friends and family close
Your friends and family can provide a crucial support network for you during your cancer treatment.
As you begin telling people about your breast cancer diagnosis, you'll likely get many offers for help. Think ahead about things you may want help with. Examples include listening when you want to talk or helping you with preparing meals.
Preparing for an appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you. If an exam or imaging test shows that you might have ductal carcinoma in situ, also called DCIS, your healthcare team will likely refer you to a specialist.
Specialists who care for people with DCIS include:
- Breast health specialists.
- Breast surgeons.
- Doctors who specialize in diagnostic tests, such as mammograms, called radiologists.
- Doctors who specialize in treating cancer, called oncologists.
- Doctors who treat cancer with radiation, called radiation oncologists.
- Genetic counselors.
- Plastic surgeons.
Here's some information to help you get ready for your appointment.
What you can do
- Write down your medical history, including any benign breast conditions with which you've been diagnosed. Also mention any radiation therapy you may have received, even years ago.
- Write down your family history of cancer. Note any family members who have had cancer. Note how each member is related to you, the type of cancer, the age at diagnosis and whether each person survived.
- Make a list of all medicines, vitamins or supplements that you're taking. If you're currently taking or have previously taken hormone replacement therapy, tell your healthcare provider.
- Consider taking a family member or friend along. Sometimes it can be difficult to absorb all the information provided during an appointment. Someone who comes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare professional.
Questions to ask your doctor
Your time with your healthcare professional is limited. Prepare a list of questions so that you can make the most of your time together. List your questions from most important to least important in case time runs out. For breast cancer, some basic questions to ask include:
- Do I have breast cancer?
- What tests do I need to determine the type and stage of cancer?
- What treatment approach do you recommend?
- What are the possible side effects or complications of this treatment?
- In general, how effective is this treatment?
- Am I a candidate for tamoxifen?
- Am I at risk of this condition recurring?
- Am I at risk of developing invasive breast cancer?
- How will you treat DCIS if it returns?
- How often will I need follow-up visits after I finish treatment?
- What lifestyle changes can help reduce my risk of a DCIS recurrence?
- Do I need a second opinion?
- Should I see a genetic counselor?
In addition to the questions that you've prepared, don't hesitate to ask other questions you think of during your appointment.
What to expect from your doctor
Be prepared to answer some questions about your symptoms and your health, such as:
- Have you gone through menopause?
- Are you using or have you used any medicines or supplements to relieve the symptoms of menopause?
- Have you had other breast biopsies or operations?
- Have you been diagnosed with any breast conditions, including noncancerous conditions?
- Have you been diagnosed with any other medical conditions?
- Do you have any family history of breast cancer?
- Have you or your female blood relatives ever been tested for BRCA gene mutations?
- Have you ever had radiation therapy?
- What is your typical daily diet, including alcohol intake?
- Are you physically active?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


