Overview
Diabetic nephropathy is a serious complication of type 1 diabetes and type 2 diabetes. It's also called diabetic kidney disease. In the United States, about 1 in 3 people living with diabetes have diabetic nephropathy.
Diabetic nephropathy affects the kidneys' usual work of removing waste products and extra fluid from the body. The best way to prevent or delay diabetic nephropathy is by living a healthy lifestyle and keeping diabetes and high blood pressure managed.
Over years, diabetic nephropathy slowly damages the kidneys' filtering system. Early treatment may prevent this condition or slow it and lower the chance of complications.
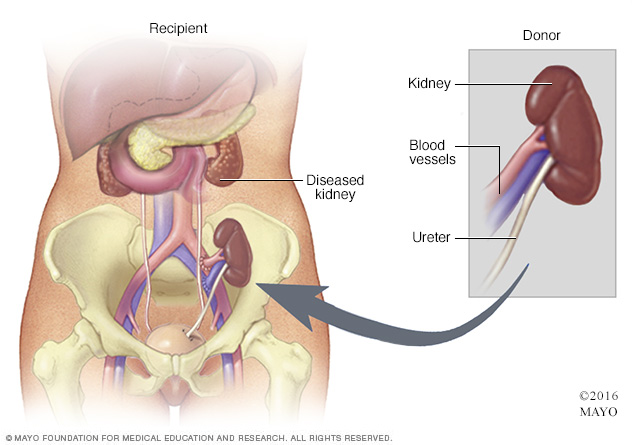
Diabetic kidney disease can lead to kidney failure. This also is called end-stage kidney disease. Kidney failure is a life-threatening condition. Treatment options for kidney failure are dialysis or a kidney transplant.
Symptoms
In the early stages of diabetic nephropathy, there might not be symptoms. In later stages, symptoms may include:
- High blood pressure that gets harder to control.
- Swelling of feet, ankles, hands or eyes.
- Foamy urine.
- Confusion or difficulty thinking.
- Shortness of breath.
- Loss of appetite.
- Nausea and vomiting.
- Itching.
- Tiredness and weakness.
When to see a doctor
Make an appointment with your health care professional if you have symptoms of kidney disease. If you have diabetes, visit your health care professional yearly or as often as you're told for tests that measure how well your kidneys are working.
Causes
Diabetic nephropathy happens when diabetes damages blood vessels and other cells in the kidneys.
How the kidneys work
The kidneys have millions of tiny blood vessel clusters called glomeruli. Glomeruli filter waste from the blood. Damage to these blood vessels can lead to diabetic nephropathy. The damage can keep the kidneys from working as they should and lead to kidney failure.
Diabetic nephropathy causes
Diabetic nephropathy is a common complication of type 1 and type 2 diabetes.
Over time, diabetes that isn't well controlled can damage blood vessels in the kidneys that filter waste from the blood. This can lead to kidney damage and cause high blood pressure.
High blood pressure can cause more kidney damage by raising the pressure in the filtering system of the kidneys.

Risk factors
If you have diabetes, the following can raise your risk of diabetic nephropathy:
- Uncontrolled high blood sugar, also called hyperglycemia.
- Uncontrolled high blood pressure, also called hypertension.
- Smoking.
- High blood cholesterol.
- Obesity.
- A family history of diabetes and kidney disease.
Complications
Complications of diabetic nephropathy can come on slowly over months or years. They may include:
- Body fluid buildup. This could lead to swelling in the arms and legs, high blood pressure, or fluid in the lungs, called pulmonary edema.
- A rise in the levels of the mineral potassium in the blood, called hyperkalemia.
- Heart and blood vessel disease, also called cardiovascular disease. This could lead to a stroke.
- Fewer red blood cells to carry oxygen. This condition also is called anemia.
- Pregnancy complications that carry risks for the pregnant person and the growing fetus.
- Damage to the kidneys that can't be fixed. This is called end-stage kidney disease. Treatment is either dialysis or a kidney transplant.
Prevention
To lower your risk of developing diabetic nephropathy:
- See your health care team regularly to manage diabetes. Keep appointments to check on how well you are managing your diabetes and to check for diabetic nephropathy and other complications. Your appointments might be yearly or more often.
- Treat your diabetes. With good treatment of diabetes, you can keep your blood sugar levels in the target range as much as possible. This may prevent or slow diabetic nephropathy.
- Manage high blood pressure or other medical conditions. If you have high blood pressure or other conditions that raise your risk of kidney disease, work with your health care professional to control them.
- Take medicines you get without a prescription only as directed. Read the labels on the pain relievers you take. This might include aspirin and nonsteroidal anti-inflammatory drugs, such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others). For people with diabetic nephropathy, these types of pain relievers can lead to kidney damage.
- Stay at a healthy weight. If you're at a healthy weight, work to stay that way by being physically active most days of the week. If you need to lose weight, talk with a member of your health care team about the best way for you to lose weight.
- Don't smoke. Cigarette smoking can damage kidneys or make kidney damage worse. If you're a smoker, talk to a member of your health care team about ways to quit. Support groups, counseling and some medicines might help.
Diagnosis
Diabetic nephropathy usually is diagnosed during the regular testing that's part of managing diabetes. Get tested every year if you have type 2 diabetes or have had type 1 diabetes for more than five years.
Routine screening tests may include:
- Urinary albumin test. This test can detect a blood protein called albumin in urine. Typically, the kidneys don't filter albumin out of the blood. Too much albumin in your urine can mean that the kidneys aren't working well.
- Albumin/creatinine ratio. Creatinine is a chemical waste product that healthy kidneys filter out of the blood. The albumin/creatinine ratio measures how much albumin compared to creatinine is in a urine sample. It shows how well the kidneys are working.
- Glomerular filtration rate (GFR). The measure of creatinine in a blood sample may be used to see how quickly the kidneys filter blood. This is called the glomerular filtration rate. A low rate means the kidneys aren't working well.
Other diagnostic tests may include:
- Imaging tests. X-rays and ultrasound can show the makeup and size of the kidneys. CT and MRI scans can show how well blood is moving within the kidneys. You may need other imaging tests, as well.
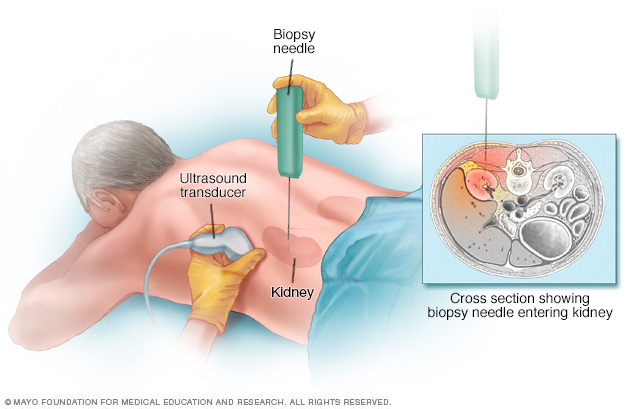
- Kidney biopsy. This is a procedure to take a sample of kidney tissue to be studied in a lab. It involves a numbing medicine called a local anesthetic. A thin needle is used to remove small pieces of kidney tissue.
Treatment
The first step in treating diabetic nephropathy is to treat and control diabetes and high blood pressure. Treatment includes diet, lifestyle changes, exercise and prescription medicines. Controlling blood sugar and blood pressure might prevent or delay kidney issues and other complications.
Medications
In the early stages of diabetic nephropathy, your treatment might include medicines to manage the following:
- Blood pressure. Medicines called angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs) are used to treat high blood pressure.
-
Blood sugar. Medicines can help control high blood sugar in people with diabetic nephropathy. They include older diabetes medicines such as insulin. Newer drugs include Metformin (Fortamet, Glumetza, others), glucagon-like peptide 1 (GLP-1) receptor agonists and SGLT2 inhibitors.
Ask your health care professional if treatments such as SGLT2 inhibitors or GLP-1 receptor agonists might work for you. These treatments can protect the heart and kidneys from damage due to diabetes.
- High cholesterol. Cholesterol-lowering drugs called statins are used to treat high cholesterol and lower the amount of protein in urine.
- Kidney scarring. Finerenone (Kerendia) might help reduce tissue scarring in diabetic nephropathy. Research has shown that the medicine might lower the risk of kidney failure. It also may lower the risk of dying from heart disease, having heart attacks and needing to go to a hospital to treat heart failure in adults with chronic kidney disease linked to type 2 diabetes.
If you take these medicines, you'll need regular follow-up testing. The testing is done to see if your kidney disease is stable or getting worse.
Treatment for advanced diabetic nephropathy
For kidney failure, also called end-stage kidney disease, treatment focuses on either replacing the work of your kidneys or making you more comfortable. Options include:
-
Kidney dialysis. This treatment removes waste products and extra fluid from the blood. Hemodialysis filters blood outside the body using a machine that does the work of the kidneys. For hemodialysis, you might need to visit a dialysis center about three times a week. Or you might have dialysis done at home by a trained caregiver. Each session takes 3 to 5 hours.
Peritoneal dialysis uses the inner lining of the abdomen, called the peritoneum, to filter waste. A cleansing fluid flows through a tube to the peritoneum. This treatment can be done at home or at work. But not everyone can use this method of dialysis.
- Transplant. Sometimes, a kidney transplant or a kidney-pancreas transplant is the best treatment choice for kidney failure. If you and your health care team decide on a transplant, you'll be assessed to find out if you can have the surgery.
- Symptom management. If you have kidney failure and you don't want dialysis or a kidney transplant, you'll likely live only a few months. Treatment may help keep you comfortable.
Potential future treatments
In the future, people with diabetic nephropathy may benefit from treatments being developed using techniques that help the body repair itself, called regenerative medicine. These techniques may help reverse or slow kidney damage.
For example, some researchers think that if a person's diabetes can be cured by a future treatment such as pancreas islet cell transplant or stem cell therapy, the kidneys might work better. These therapies, as well as new medicines, are still being studied.
Lifestyle and home remedies
Diet, exercise and self-care are needed to control blood sugar and high blood pressure. Your diabetes care team can help you with the following goals:
- Monitor your blood sugar. Your health care team will tell you how often to check your blood sugar level to make sure you stay in your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to check your blood sugar level several times a day.
- Be active most days of the week. Aim for at least 30 minutes or more of moderate to vigorous aerobic exercise on most days. Go for a total of at least 150 minutes a week. Activities might include brisk walking, swimming, biking or running.
- Eat a healthy diet. Eat a high-fiber diet with lots of fruits, nonstarchy vegetables, whole grains and legumes. Limit saturated fats, processed meats, sweets and salt.
- Quit smoking. If you smoke, talk with your health care professional about ways to quit.
- Stay at a healthy weight. If you need to lose weight, talk with your health care professional about ways to do so. For some people, weight-loss surgery is an option.
- Take a daily aspirin. Talk with your health care professional about whether you should take a daily low-dose aspirin to lower the risk of heart disease.
- Talk to your health care team. Make sure all your health care professionals know that you have diabetic nephropathy. They can take steps to protect your kidneys from more damage by not doing medical tests that use contrast dye. These include angiograms and computerized tomography (CT) scans.
Coping and support
If you have diabetic nephropathy, these steps may help you cope:
- Connect with other people who have diabetes and kidney disease. Ask a member of your health care team about support groups in your area. Or contact groups such as the American Association of Kidney Patients or the National Kidney Foundation for groups in your area.
- Stick to your usual routine, when possible. Try to keep your usual routine, doing the activities you enjoy and working, if your condition allows. This may help you cope with feelings of sadness or loss that you may have after your diagnosis.
- Talk with someone you trust. Living with diabetic nephropathy can be stressful, and it may help to talk about your feelings. You may have a friend or family member who is a good listener. Or you may find it helpful to talk with a faith leader or someone else you trust. Ask a member of your health care team for the name of a social worker or counselor.
Preparing for an appointment
Diabetic nephropathy most often is found during regular appointments for diabetes care. If you've been diagnosed with diabetic nephropathy recently, you may want to ask your health care professional the following questions:
- How well are my kidneys working now?
- How can I keep my condition from getting worse?
- What treatments do you suggest?
- How do these treatments change or fit into my diabetes treatment plan?
- How will we know if these treatments are working?
Questions for ongoing appointments
Before any appointment with a member of your diabetes treatment team, ask whether you need to follow any restrictions, such as fasting before taking a test. Questions to regularly review with your doctor or other members of the team include:
- How often should I check my blood sugar? What is my target range?
- What changes in my diet would help me better manage my blood sugar, cholesterol or blood pressure?
- When should I take my medicines? Do I take them with food?
- How does managing my diabetes affect treatment for other conditions I have? How can I manage my treatments better?
- When do I need to make a follow-up appointment?
- What should prompt me to call you or seek emergency care?
- Are there brochures or online sources you can suggest?
- Is there help for paying for diabetes supplies?
What to expect from your doctor
Your health care professional is likely to ask you questions during your appointments, including:
- Do you understand your treatment plan and know that you can follow it?
- How are you coping with diabetes?
- Have you had any low blood sugar?
- Do you know what to do if your blood sugar is too low or too high?
- What do you usually eat in a day?
- Are you exercising? If so, what type of exercise? How often?
- Do you sit a lot?
- What are you finding hard about managing your diabetes?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


