Overview
Cushing syndrome happens when the body has too much of the hormone cortisol for a long time. This can result from the body making too much cortisol, or from taking medicines called glucocorticoids, which affect the body the same way as cortisol.
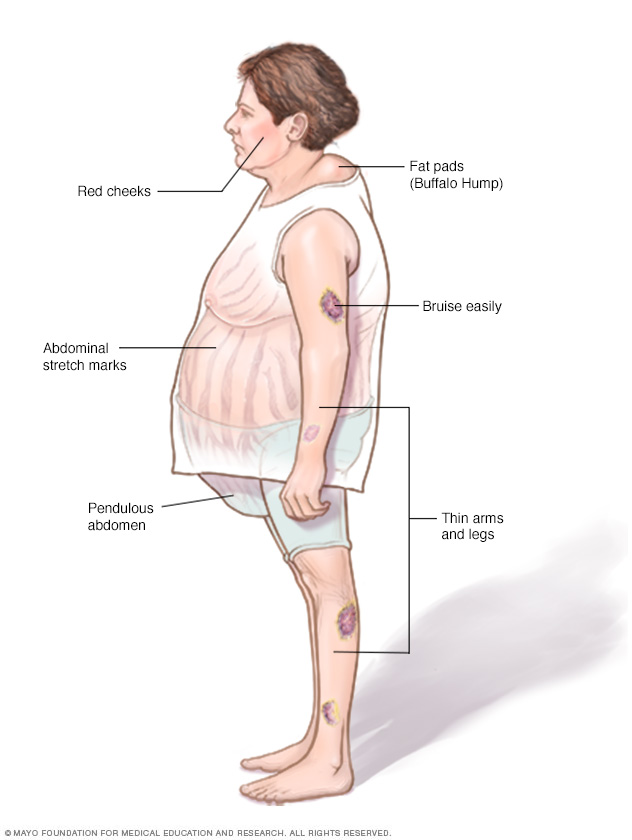
Too much cortisol can cause some of the main symptoms of Cushing syndrome — a fatty hump between the shoulders, a rounded face, and pink or purple stretch marks on the skin. Cushing syndrome also can cause high blood pressure or bone loss. Sometimes, it can cause type 2 diabetes.
Treatments for Cushing syndrome can lower the body's cortisol levels and improve symptoms. The sooner treatment starts, the better the chances for recovery.
Symptoms
Symptoms of Cushing syndrome can vary depending on the level of extra cortisol.
Common symptoms of Cushing syndrome
- Weight gain in the trunk, with thin arms and legs.
- Weight gain in the face. This is sometimes called moon face.
- A fatty lump between the shoulders. This may be referred to as a buffalo hump.
- Pink or purple stretch marks on the stomach, hips, thighs, breasts and underarms.
- Thin, frail skin that bruises easily.
- Slow wound healing.
- Acne.
Symptoms women with Cushing syndrome may experience
- Thick, dark hair on the face and body. This condition is called hirsutism.
- Periods that are irregular or that stop.
Symptoms men with Cushing syndrome may experience
- Lower sex drive.
- Reduced fertility.
- Problems getting an erection.
Other possible symptoms of Cushing syndrome
- Extreme tiredness.
- Muscle weakness.
- Depression, anxiety and irritability.
- Emotions that are hard to control.
- Trouble concentrating or remembering.
- Sleeplessness.
- High blood pressure.
- Headache.
- Infections.
- Skin darkening.
- Bone loss, which can lead to broken bones.
- Stunted growth in children.
When to see a doctor
Call your health care provider if you have symptoms of Cushing syndrome, especially if you're taking glucocorticoid medicine to treat a health issue such as asthma, arthritis or inflammatory bowel disease.
Causes
Cushing syndrome is caused by having too much cortisol in the body. Cortisol is a hormone that is made in the adrenal glands. It helps the body respond to stress and plays many other important roles, including:
- Controlling blood pressure.
- Reducing inflammation.
- Helping the heart and blood vessels work correctly.
- Controlling blood sugar.
- Helping the body use food for energy.
The role of glucocorticoid medicines (exogenous Cushing syndrome)
Cushing syndrome can happen from taking glucocorticoid medicines. These are often used to treat inflammatory diseases such as rheumatoid arthritis, lupus and asthma. Pain or injury in the back or joints and many skin rashes may be treated with glucocorticoids. They also may be used to stop the body from rejecting a new organ after a transplant.
Glucocorticoids may be taken by mouth, given as a shot, rubbed into the skin or breathed into the lungs by an inhaler. Any form of glucocorticoid, if taken in large amounts for a long time, can cause Cushing syndrome.
When the body makes too much cortisol (endogenous Cushing syndrome)
A hormone made in the pituitary gland controls how much cortisol the body makes. This is called adrenocorticotropic hormone (ACTH). Some tumors make ACTH, which creates more cortisol and can cause Cushing syndrome. Problems with the adrenal glands also can affect cortisol and cause Cushing syndrome.
When Cushing syndrome happens this way, it may be caused by:
- ACTH-producing pituitary adenoma. Pituitary adenomas are tumors that grow in the pituitary gland. They are found at the base of the brain and are usually not cancer. These tumors sometimes make too much ACTH. This causes the adrenal glands to make extra cortisol. When Cushing syndrome happens this way, it's called Cushing disease. It happens more often in women and is the most common type of endogenous Cushing syndrome.
- Ectopic ACTH-producing tumor. Rarely, a tumor that makes too much ACTH grows in an organ that usually doesn't make ACTH. This is called ectopic ACTH production. It causes the body to make too much cortisol. These tumors can be cancerous, but aren't always. They are usually found in the lungs, pancreas, thyroid or thymus gland.
-
Adrenal gland tumors or disease. Problems with the adrenal glands can cause them to make too much cortisol. The most common is a tumor in the outer part of the adrenal gland called an adrenal adenoma. These tumors are not cancer, and only some make too much cortisol.
Cancerous tumors in the outer part of the adrenal glands, known as adrenocortical carcinoma, are rare. But they can make cortisol and cause Cushing syndrome. Sometimes, several lumps that make cortisol can grow in the adrenal glands and cause Cushing syndrome. This is called adrenal nodular hyperplasia.
- Familial Cushing syndrome. Rarely, people inherit a tendency to get tumors on one or more of their endocrine glands, which are glands that make hormones. If these tumors make ACTH or cortisol, Cushing syndrome can happen.

Complications
Without treatment, Cushing syndrome can cause complications, including:
- Bone loss, also called osteoporosis, which can lead to broken bones.
- High blood pressure, also called hypertension.
- Type 2 diabetes.
- Serious or multiple infections.
- Loss of muscle mass and strength.
Diagnosis
Taking glucocorticoid medicines is the most common way to get Cushing syndrome. Your health care provider can look at all your medicines — pills, injections, creams and inhalers — to see if you're taking medicines that can cause the syndrome. If you are, you won't need other tests.
When Cushing syndrome is caused by the body making too much cortisol, it can be hard to diagnose. That's because other illnesses have similar symptoms. Diagnosing Cushing syndrome can be a long and complex process. You'll need to see a doctor who specializes in hormonal diseases, called an endocrinologist.
The endocrinologist likely will do a physical exam and look for signs of Cushing syndrome, such as a round face, a hump on the back of the neck, and thin, bruised skin with stretch marks.
If you haven't been using a glucocorticoid medicine, these tests may help pinpoint the cause of Cushing syndrome:
-
Urine and blood tests. These tests measure hormone levels and show if the body is making too much cortisol. For the urine test, you may be asked to collect your urine over a 24-hour period. Cortisol, ACTH and other hormones are be measured in urine and blood samples.
Your health care provider also might recommend other tests. These tests measure cortisol levels before and after using hormone medicines to trigger or block cortisol.
- Saliva test. Cortisol levels typically rise and fall during the day. In people without Cushing syndrome, cortisol drops in the evening. By looking at cortisol levels from a small sample of saliva collected at night, the health care team can see if cortisol levels are too high.
- Imaging tests. CT or MRI scans can take pictures of the pituitary and adrenal glands to see if anything shows up, such as tumors.
-
Inferior petrosal sinus sampling. This test can help decide if Cushing syndrome is caused by an ACTH-producing pituitary adenoma, or ACTH-producing tumor in another organ. For the test, blood samples are taken from the veins that drain the pituitary gland, called the inferior petrosal sinuses.
During the test, you are given medicine through a vein to help you stay calm and comfortable. A thin tube is placed in your groin or neck area and is threaded to the inferior petrosal sinuses to collect a blood sample. Another blood sample is taken from your forearm. You are then given a medicine that causes the tumor to make more ACTH, and blood samples are taken again from the same areas. Levels of ACTH are then compared between the two sample areas.
If the ACTH level is higher in the sinus sample, the problem is coming from the pituitary. If the ACTH levels are similar between the sinuses and forearm, the problem is outside of the pituitary gland.
These tests help your health care provider diagnose Cushing syndrome. They also may help rule out other health conditions, such as polycystic ovary syndrome — a hormone problem in people with enlarged ovaries. Depression, eating disorders and alcoholism also can have symptoms similar to Cushing syndrome.
Treatment
Treatments for Cushing syndrome are designed to lower the amount of cortisol in the body. The best treatment for you depends on the cause of the syndrome. Options include:
Reducing glucocorticoid use
If Cushing syndrome is caused by taking glucocorticoid medicine for a long time, your health care provider may be able to control your symptoms by lowering how much medicine you take. This is done carefully over time, while still managing the condition for which you take it. Don't reduce the dose of glucocorticoid drugs or stop taking them on your own. Do so only with help from your health care provider.
Stopping these medicines too quickly can cause you to have too little cortisol in your body. Slowly tapering off the medicine allows your body to make a healthy amount of cortisol.
Surgery
If Cushing syndrome is caused by a tumor, your health care provider may recommend removing the tumor with surgery. Pituitary tumors are often removed by a neurosurgeon, who may do the operation through your nose. ACTH-producing tumors in other parts of the body may be removed with regular surgery or using less-invasive approaches with smaller incisions.
If an ACTH-producing tumor isn't found, or if one can't be fully removed and Cushing syndrome continues, your health care provider may recommend removing the adrenal glands. This is called a bilateral adrenalectomy. This procedure immediately stops the body from making too much cortisol. After both adrenal glands are removed, you may need to take medicines to replace cortisol and another adrenal hormone called aldosterone for the rest of your life.
Adrenal gland tumors can be removed through an incision in the midsection or back. Often, adrenal gland tumors that are noncancerous can be removed with a minimally invasive approach.
After Cushing syndrome surgery, your body won't make enough ACTH. You'll need to take a cortisol replacement medicine to give your body the right amount of cortisol. Most of the time, your body starts making enough cortisol again, and your health care provider can taper off the replacement medicine. Your endocrinologist may use blood tests to help decide if you need cortisol medicine and when it may be stopped.
This process can take from six months to a year or more. Sometimes, people with Cushing syndrome need lifelong replacement medicine.
Radiation therapy
If the surgeon can't totally remove a pituitary tumor, radiation therapy may be needed along with surgery. Radiation also may be used for people who can't have surgery.
Radiation can be given in small doses over six weeks, or with a single, high dose of radiation. In both cases, your health care provider can plan your procedure in a way that reduces radiation exposure to other tissues.
Medications
Medicines can be used to control cortisol levels when surgery and radiation don't work or aren't an option. Medicines also might be used before surgery in people who are very sick with Cushing syndrome. This can improve symptoms of the disease and reduce the risks of surgery. Medical therapy for Cushing syndrome is not a cure and may not completely improve all of the symptoms of too much cortisol.
Medicines to control cortisol production at the adrenal gland include ketoconazole, osilodrostat (Isturisa), mitotane (Lysodren), levoketoconazole (Recorlev), and metyrapone (Metopirone).
Mifepristone (Korlym, Mifeprex) is approved for people with Cushing syndrome who have type 2 diabetes or high blood sugar. Mifepristone does not lower the amount of cortisol the body makes, but it blocks the effect of cortisol on tissues.
Pasireotide (Signifor) is given as a shot two times a day. It works by lowering the amount of ACTH from the tumor, which lowers cortisol levels. Other medicines are being developed.
Side effects from these medicines may include tiredness, upset stomach, vomiting, headaches, muscle aches, high blood pressure, low potassium and swelling. Some have more-serious side effects, such as brain and nervous system side effects and liver damage.
Sometimes, the tumor or its treatment causes the pituitary or adrenal gland to make too little of other hormones. If this happens, your health care provider can recommend hormone replacement.
Lifestyle and home remedies
Recovering from Cushing syndrome is usually a slow, gradual process. It can take time before you start to feel better. These tips may help you on your journey back to health.
- Increase activities slowly. Work up to a comfortable level of exercise or activity without overdoing it. Don't do activities that could cause you to get hurt, such as high-impact exercise. With patience and consistency, you'll improve little by little over time.
- Eat sensibly. Nutritious foods are a good source of fuel for your body during recovery. They also can help you lose any weight you gained from Cushing syndrome. Make sure you're getting enough calcium and vitamin D. Taken together, they help your body absorb calcium, which may strengthen your bones. This can counteract the bone density loss caused by Cushing syndrome.
- Keep an eye on your mental health. Depression can be a side effect of Cushing syndrome, but it also can continue or start after treatment begins. Don't ignore depression or wait it out. Seek help quickly from your health care provider or a therapist if you're depressed, overwhelmed or having trouble coping during your recovery.
- Gently soothe aches and pains. Hot baths, massages and low-impact exercises, such as water aerobics and tai chi, can help reduce some of the muscle and joint pain that happens during Cushing syndrome recovery.
Coping and support
Support groups can be helpful in dealing with Cushing syndrome and recovery. They bring you together with other people who have the same kinds of challenges, along with their families and friends. Support groups offer a place where you can share common problems with others who understand.
Ask your health care provider about support groups in your community. Your local health department, public library and the internet also may be good sources to find a support group in your area.
Preparing for an appointment
You're likely to see your primary care provider first. However, sometimes when you call to set up an appointment, you may be referred immediately to a doctor who specializes in hormonal disorders, called an endocrinologist.
It's a good idea to prepare for your visit. This way, you can make the most of your time with your health care provider. Here's how you can get ready, and what to expect.
What you can do
- Know what to do before your visit. When you make the appointment, ask if there's anything you need to do to prepare for testing.
- Write down any symptoms you're having, including any that seem unrelated to the appointment. For example, if you've had headaches more often or if you've been feeling down or more tired than usual, tell your health care provider. Also talk to your provider about changes in your appearance, such as weight gain, new acne or more body hair.
- Write down key personal information, including any changes in your relationships or sex life. Let your provider know if the people closest to you have noticed that you seem irritable or have more mood swings than in the past. It may help to bring a photo of yourself that shows any changes in your appearance since you've started having symptoms.
- Make a list of all medicines, vitamins, creams or supplements you're currently taking or have used in the past. Write down the name, dose and dates of any steroid medicines you've taken before, such as cortisone shots.
- Take a family member or friend along, if possible. Sometimes it can be hard to remember all the information you get during an appointment. Someone who comes with you may remember something that you missed or forgot.
- Write down questions to ask your health care provider.
Your time with your provider may be limited, so preparing a list of questions may help you make the most of your time together. For Cushing syndrome, some basic questions to ask include:
- What's causing my symptoms?
- What tests do I need? How are these tests done?
- What are my treatment options? Which do you recommend for me?
- Will my symptoms get better with treatment? Will I see a change in how I look or how I feel?
- Will treatment help me feel better emotionally?
- What is the long-term effect of each treatment? Will this affect if I can have children?
- How will you know the treatment is working?
- I have other health conditions. How can I best manage these conditions together?
- Are there any brochures or other printed materials that I can take home with me? What websites do you recommend?
In addition to the questions that you've prepared, feel free to ask any other questions during your appointment.
What to expect from your doctor
Your health care provider is likely to ask you many questions. Being ready to answer them may save time so that you can discuss other concerns or questions you have. Your provider may ask:
- When did you first have symptoms?
- Do you have symptoms all the time, or do they come and go? Have they gotten worse over time?
- Have you noticed any changes in your sexual performance or your interest in sex?
- Has your menstrual cycle changed or have you stopped having your period?
- Have you gained weight? On what part of your body?
- Have you had trouble controlling your emotions?
- Have you noticed that you bruise more easily, or that cuts and infections take longer to heal?
- Do your muscles feel weak? Is it hard to get out of the tub or walk up or down stairs?
- Have you noticed new acne or more body or facial hair?
- Have you been taking a glucocorticoid medication? For how long?
- What, if anything, makes your symptoms better or worse?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


