Overview
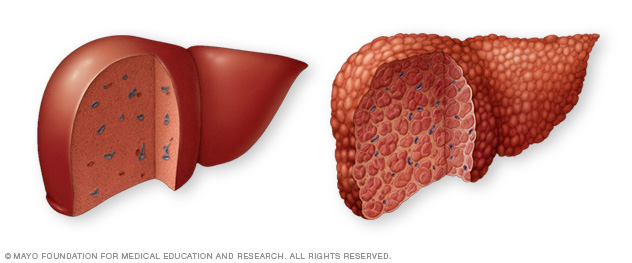
Cirrhosis is advanced scarring of the liver caused by many diseases and conditions, including hepatitis or alcohol use disorder.
Each time the liver is injured — whether by alcohol use disorder or another cause, such as infection — it tries to repair itself. In the process, scar tissue forms. As cirrhosis gets worse, more and more scar tissue forms, making it difficult for the liver to do its job. Advanced cirrhosis is life-threatening.
The liver damage caused by cirrhosis generally can't be undone. But if liver cirrhosis is diagnosed early and the underlying cause is treated, further damage can be limited. In rare cases, it may be reversed.
Symptoms
Cirrhosis often has no symptoms until liver damage is serious. When symptoms do happen, they may include:
- Extreme tiredness.
- Easily bleeding or bruising.
- Loss of appetite.
- Nausea.
- Swelling in the legs, feet or ankles, called edema.
- Weight loss.
- Itchy skin.
- Yellow discoloration in the skin and eyes, called jaundice.
- Fluid buildup in the belly, called ascites (uh-SAHY-teez).
- Spiderlike blood vessels on the skin.
- Redness in the palms of the hands.
- Pale fingernails, especially the thumb and index finger.
- Clubbing of the fingers, in which the fingertips spread out and become rounder than usual.
- For women, absence of or loss of periods not related to menopause.
- For men, loss of sex drive, testicular shrinkage or breast enlargement, known as gynecomastia.
- Confusion, drowsiness or slurred speech.
When to see a doctor
Make an appointment with a healthcare professional if you have any of the symptoms listed above.
Causes
A wide range of diseases and conditions can damage the liver and lead to cirrhosis. Some of the causes include:
- Long-term alcohol abuse.
- Ongoing viral hepatitis (hepatitis B, C and D).
- Metabolic dysfunction-associated steatotic liver disease — formerly called nonalcoholic fatty liver disease — a condition in which fat builds up in the liver.
- Hemochromatosis, a condition that causes iron buildup in the body.
- Autoimmune hepatitis, which is a liver disease caused by the body's immune system.
- Destruction of the bile ducts caused by primary biliary cholangitis.
- Hardening and scarring of the bile ducts caused by primary sclerosing cholangitis.
- Wilson's disease, a condition in which copper build up in the liver.
- Cystic fibrosis.
- Alpha-1 antitrypsin deficiency.
- Poorly formed bile ducts, a condition known as biliary atresia.
- Disorders of sugar metabolism, such as galactosemia or glycogen storage disease.
- Alagille syndrome, a genetic digestive disorder.
- Infection, such as syphilis or brucellosis.
- Medicines, including methotrexate or isoniazid.
Risk factors
- Drinking too much alcohol. Alcohol abuse is a risk factor for cirrhosis.
- Being overweight. Being obese increases the risk of conditions that may lead to cirrhosis. These conditions include metabolic dysfunction-associated steatotic liver disease, formerly called nonalcoholic fatty liver disease; and metabolic dysfunction-associated steatohepatitis, formerly called nonalcoholic steatohepatitis.
- Having viral hepatitis. Not everyone with chronic hepatitis will develop cirrhosis, but it's one of the world's leading causes of liver disease.
Complications
Complications of cirrhosis can include:
- High blood pressure in the veins that supply the liver. This condition is known as portal hypertension. Cirrhosis slows the regular flow of blood through the liver. This increases pressure in the vein that brings blood to the liver.
- Swelling in the legs and belly. The increased pressure in the portal vein can cause fluid to build up in the legs, called edema, and in the belly, called ascites. Edema and ascites also may happen if the liver can't make enough of certain blood proteins, such as albumin.
- Swelling of the spleen. Portal hypertension can cause the spleen to trap white blood cells and platelets. This makes the spleen swell, a condition known as splenomegaly. Fewer white blood cells and platelets in your blood can be the first sign of cirrhosis.
- Bleeding. Portal hypertension can cause blood to be redirected to smaller veins. Strained by the extra pressure, these smaller veins can burst, causing serious bleeding. Portal hypertension also may cause enlarged veins, called varices (VAIR-uh-seez), in the esophagus or the stomach. These varices also may lead to life-threatening bleeding. If the liver can't make enough clotting factors, this also can contribute to continued bleeding.
- Infections. Having cirrhosis makes it hard for the body to fight infections. Ascites also can lead to bacterial peritonitis, a serious infection.
- Malnutrition. Cirrhosis may make it more difficult for the body to process nutrients, leading to weakness and weight loss.
- Buildup of toxins in the brain. A liver damaged by cirrhosis can't clear toxins from the blood as well as a healthy liver can. These toxins can then build up in the brain and cause mental confusion and difficulty concentrating. This is known as hepatic encephalopathy. With time, hepatic encephalopathy can progress to unresponsiveness or coma.
- Jaundice. Jaundice happens when the diseased liver doesn't remove enough bilirubin, a blood waste product, from the blood. Jaundice causes yellowing of the skin and whites of the eyes and darkening of urine.
- Bone disease. Some people with cirrhosis lose bone strength and are at greater risk of fractures.
- Increased risk of liver cancer. A large proportion of people who develop liver cancer have pre-existing cirrhosis.
- Acute-on-chronic cirrhosis. Some people end up experiencing multiorgan failure. Researchers now believe this is a complication in some people who have cirrhosis. However, they don't fully understand what causes it.
Prevention
Lower the risk of cirrhosis by taking these steps to care for your liver:
- Do not drink alcohol if you have cirrhosis. If you have liver disease, you should not drink alcohol.
- Eat a healthy diet. Choose a diet that's full of fruits and vegetables. Select whole grains and lean sources of protein. Cut down on the amount of fatty and fried foods you eat.
- Maintain a healthy weight. Too much body fat can damage the liver. Talk to a healthcare professional about a weight-loss plan if you are obese or overweight.
- Reduce your risk of hepatitis. Sharing needles and having unprotected sex can increase the risk of hepatitis B and C. Ask a care professional about hepatitis vaccinations.
If you're concerned about your risk of liver cirrhosis, talk to a health professional about ways to reduce your risk.
Diagnosis
People with early-stage cirrhosis of the liver usually don't have symptoms. Often, cirrhosis is first found through a routine blood test or checkup. To help confirm a diagnosis, a combination of laboratory and imaging tests is usually done.
Tests
A healthcare professional may order one or more tests to check liver function, including:
-
Lab tests. A healthcare professional may order blood tests to check for signs of liver malfunction, such as high bilirubin levels or certain enzymes. To evaluate kidney function, the blood is checked for creatinine. A blood count would be measured and blood is screened for hepatitis viruses. An international normalized ratio (INR) also is checked for the blood's ability to clot.
Based on history and blood test results, a medical professional may be able to diagnose the underlying cause of cirrhosis. Blood tests also can help identify the stage of cirrhosis.
- Imaging tests. Certain imaging tests, including transient or magnetic resonance elastography (MRE), may be recommended. These noninvasive imaging tests look for hardening or stiffening of the liver. Other imaging tests, such as MRI, CT and ultrasound, also may be done.
- Biopsy. A tissue sample, called a biopsy, is not necessarily needed for diagnosis. However, it may be done to find out how severe liver damage is and what's causing it.
If you have cirrhosis, a healthcare professional is likely to recommend regular tests to see if liver disease has progressed or check for signs of complications, especially esophageal varices and liver cancer. Noninvasive tests are becoming more widely available for keeping an eye on liver disease.

Treatment
Treatment for cirrhosis depends on the cause and extent of liver damage. The goals of treatment are to slow the progression of scar tissue in the liver and to prevent or treat symptoms and complications of cirrhosis. For severe liver damage, hospitalization may be needed.
Treatment for the underlying cause of cirrhosis
In early cirrhosis, it may be possible to minimize damage to the liver by treating the underlying cause. The options include:
- Treatment for alcohol dependency. People with cirrhosis caused by excessive alcohol use should try to stop drinking. If stopping alcohol use is difficult, a healthcare professional may recommend a treatment program for alcohol addiction. For people with cirrhosis, it is very important to stop drinking since any amount of alcohol is toxic to the liver.
- Weight loss. People with cirrhosis caused by metabolic dysfunction-associated steatotic liver disease may become healthier if they lose weight and control their blood sugar levels.
- Medicines to control hepatitis. Medicines may limit further damage to liver cells caused by hepatitis B or C through specific treatment of these viruses.
- Medicines to control other causes and symptoms of cirrhosis. Medicines may slow the progression of certain types of liver cirrhosis. For example, for people with primary biliary cholangitis that is diagnosed early, medicine may significantly delay progression to cirrhosis.
Other medicines can relieve certain symptoms, such as itching, fatigue and pain. Nutritional supplements may be prescribed to treat malnutrition associated with cirrhosis. Supplements also can help prevent weak bones, known as osteoporosis.
Treatment for complications of cirrhosis
A healthcare professional will work to treat any complications of cirrhosis, including:
- A buildup of fluid in the body. A low-sodium diet and medicine to prevent fluid buildup in the body may help control ascites and swelling. More-severe fluid buildup may need procedures to drain the fluid or surgery to relieve pressure.
-
Portal hypertension. Certain blood pressure medicines may control increased pressure in the veins that supply the liver, called portal hypertension, and prevent severe bleeding. An upper endoscopy may be done on a regular basis to look for enlarged veins in the esophagus or stomach that may bleed. These veins are known as varices.
If someone develops varices, medicine will likely be prescribed to lower the risk of bleeding. If there are signs that the varices are bleeding or are likely to bleed, a procedure known as band ligation may be needed. Band ligation can stop the bleeding or reduce the risk of further bleeding. In severe cases, a small tube called a transjugular intrahepatic portosystemic shunt may be placed in the vein to reduce blood pressure in the liver.
- Infections. Antibiotics or other treatments for infections may be needed. A healthcare professional also is likely to recommend vaccinations for influenza, pneumonia and hepatitis.
- Increased liver cancer risk. A healthcare professional will likely recommend regular blood tests and ultrasound exams to look for signs of liver cancer.
- Hepatic encephalopathy. Some people may be prescribed medicines to help reduce the buildup of toxins in the blood caused by poor liver function.
Liver transplant surgery
In advanced cases of cirrhosis, when the liver stops working properly, a liver transplant may be the only treatment option. A liver transplant is a procedure to replace the liver with a healthy liver from a deceased donor or with part of a liver from a living donor. Cirrhosis is one of the most common reasons for a liver transplant. Candidates for liver transplant have extensive testing to determine whether they are healthy enough to have a good outcome following surgery.
Historically, those with alcoholic cirrhosis have not been liver transplant candidates because of the risk that they will return to harmful drinking after transplant. Recent studies, however, suggest that carefully selected people with severe alcoholic cirrhosis have posttransplant survival rates similar to those of liver transplant recipients with other types of liver disease.
For transplant to be an option if you have alcoholic cirrhosis, you would need to:
- Find a program that works with people who have alcoholic cirrhosis.
- Meet the requirements of the program. These would include lifelong commitment to alcohol abstinence as well as other requirements of the specific transplant center.
Potential future treatments
Scientists are working to expand current treatments for cirrhosis, but success has been limited. Because cirrhosis has a variety of causes and complications, there are many potential avenues of approach. A combination of increased screening, lifestyle changes and new medicines may improve outcomes for people with liver damage, if started early.
Researchers are working on therapies that will specifically target liver cells, helping to slow or even reverse the fibrosis that leads to cirrhosis. However, no targeted therapy is quite ready.
Lifestyle and home remedies
If you have cirrhosis, be careful to limit additional liver damage:
- Don't drink alcohol. Whether your cirrhosis was caused by chronic alcohol use or another disease, don't drink alcohol. Drinking alcohol may cause further liver damage.
- Eat a low-sodium diet. Excess salt can cause your body to retain fluids, worsening swelling in your abdomen and legs. Use herbs for seasoning your food, rather than salt. Choose prepared foods that are low in sodium.
- Eat a healthy diet. People with cirrhosis can experience malnutrition. Combat this with a healthy diet that includes a variety of fruits and vegetables. Choose lean protein, such as legumes, poultry or fish. Don't eat raw seafood.
- Protect yourself from infections. Cirrhosis makes it more difficult for you to fight off infections. Protect yourself by avoiding people who are sick and washing your hands frequently. Get vaccinated for hepatitis A and B, influenza, and pneumonia.
- Use over-the-counter medicines carefully. Cirrhosis makes it more difficult for your liver to process medicines. For this reason, ask a healthcare professional before taking any medicines, including nonprescription ones. Don't take aspirin and ibuprofen (Advil, Motrin IB, others). If you have liver damage, a care professional may recommend that you not take acetaminophen (Tylenol, others) or take it in low doses for pain relief.
Preparing for an appointment
If you have cirrhosis, you may be referred to a healthcare professional who specializes in the digestive system, called a gastroenterologist, or the liver, called a hepatologist.
Here's some information to help you get ready for your appointment and what to expect.
What you can do
- Be aware of any pre-appointment restrictions, such as diet restrictions on the day before your appointment.
- Write down your symptoms, including when they started and how they may have changed or worsened over time.
- Take a list of all your medicines, as well as any vitamins or supplements.
- Write down your key medical information, including other diagnosed conditions.
- Bring results of medical tests done so far, including digital copies of CT, MRI, or ultrasound images and biopsy slides if a liver biopsy has been done.
- Write down key personal information, including any recent changes or stressors in your life.
- Take a family member or friend along to help you remember things.
- Write down questions to ask your doctor.
Questions to ask your doctor
Preparing a list of questions can help you make the most of your time. Some basic questions to ask include:
- What is most likely causing my cirrhosis?
- Is there a way to slow or stop my liver damage?
- What are my treatment options?
- Are there medicines or supplements that can hurt my liver?
- What signs and symptoms of complications should I watch for?
- I have other health conditions. How can I best manage them together?
Don't hesitate to ask additional questions during your appointment.
What to expect from your doctor
Be prepared to answer questions, including:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- How often do you drink alcohol?
- Have you been exposed to or taken toxic drugs?
- Do you have a family history of liver disease, hemochromatosis or obesity?
- Have you ever had viral hepatitis?
- Have you ever had jaundice?
- Have you ever had a blood transfusion or used injected drugs?
- Do you have any tattoos?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


