Overview
Chronic myelogenous leukemia, also called CML, is an uncommon type of cancer of the bone marrow. Bone marrow is the spongy tissue inside bones where blood cells are made. CML causes an increased number of white blood cells in the blood.
The term "chronic" in chronic myelogenous leukemia means this cancer tends to progress more slowly than severe forms of leukemia. The term "myelogenous" (my-uh-LOHJ-uh-nus) refers to the type of cells affected by this cancer.
Chronic myelogenous leukemia also can be called chronic myeloid leukemia and chronic granulocytic leukemia. It typically affects older adults and rarely occurs in children, though it can occur at any age.
Advances in treatment have improved the prognosis of people with chronic myelogenous leukemia. Most people can achieve remission and live for many years after diagnosis.
Symptoms
Chronic myelogenous leukemia often doesn't cause symptoms. It might be detected during a blood test.
When they occur, symptoms may include:
- Bone pain.
- Bleeding easily.
- Feeling full after eating a small amount of food.
- Fatigue.
- Fever.
- Weight loss without trying.
- Loss of appetite.
- Pain or fullness below the ribs on the left side.
- Excessive sweating during sleep.
- Blurry vision caused by bleeding in the back of the eye.
Overview
When to see a doctor
Make an appointment with your health care provider if you have any persistent symptoms that worry you.
Causes
Chronic myelogenous leukemia happens when something causes changes to the bone marrow cells. It's not clear what starts this process. However, doctors have discovered how it progresses into chronic myelogenous leukemia.
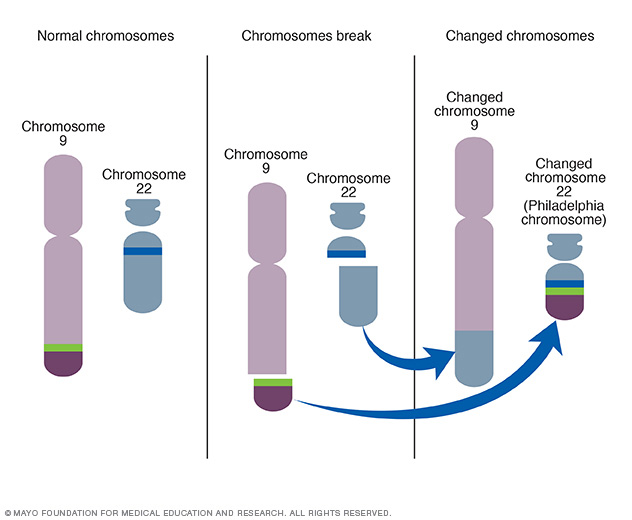
A new chromosome develops
Human cells typically have 23 pairs of chromosomes. These chromosomes hold the DNA that contains the instructions that tell the cells what to do. In people with chronic myelogenous leukemia, the chromosomes in the blood cells swap sections with each other. A section of chromosome 9 switches places with a section of chromosome 22. This creates an extra-short chromosome 22 and an extra-long chromosome 9.
The extra-short chromosome 22 is called the Philadelphia chromosome. It is named for the city where it was discovered. The Philadelphia chromosome is present in the blood cells of 90% of people with chronic myelogenous leukemia.
The Philadelphia chromosome creates a new gene
Genes from chromosome 9 combine with genes from chromosome 22 to create a new gene called BCR-ABL. The BCR-ABL gene tells the blood cells to produce too much of a protein called tyrosine kinase. Tyrosine kinase promotes cancer by allowing certain blood cells to grow out of control.
The new gene allows too many diseased blood cells
Blood cells begin growing in the bone marrow. When the bone marrow functions correctly, it produces immature cells, called blood stem cells, in a controlled way. These cells then mature and specialize into the red cells, white cells and platelets that circulate in the blood.
In chronic myelogenous leukemia, this process doesn't work properly. The tyrosine kinase allows too many white blood cells to grow. Most or all of these cells contain the Philadelphia chromosome. The diseased white blood cells don't grow and die like they should. The diseased white blood cells build up in huge numbers. They crowd out healthy blood cells and damage the bone marrow.
Risk factors
Factors that increase the risk of chronic myelogenous leukemia include:
- Older age. CML is more common in older people than in children and teens.
- Being male. Men are slightly more at risk of developing CML than are women.
- Radiation exposure. Radiation therapy for certain types of cancer has been linked to CML.
There's no way to prevent chronic myelogenous leukemia. If you get it, there's nothing you could have done to prevent it.
Family history is not a risk factor
The gene change that leads to chronic myelogenous leukemia isn't passed from parents to children. This change is believed to develop after birth.
Diagnosis
Tests and procedures used to diagnose chronic myelogenous leukemia include:
- Physical exam. Your health care provider examines you and checks vital signs such as pulse and blood pressure. Your provider also feels your lymph nodes, spleen and abdomen for swelling.
- Blood tests. A sample of blood is drawn using a needle. The sample is sent to a lab for a complete blood count, also called a CBC. A CBC checks the number of different types of cells in the blood. Chronic myelogenous leukemia often causes a very high number of white blood cells. Blood tests also can measure organ function to show if anything isn't working properly.
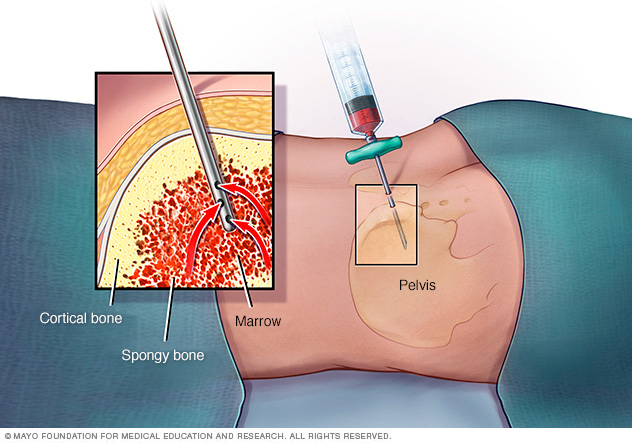
- Bone marrow tests. Bone marrow biopsy and bone marrow aspiration are used to collect bone marrow samples for testing. Bone marrow has a solid and a liquid part. In a bone marrow biopsy, a needle is used to collect a small amount of the solid tissue. In a bone marrow aspiration, a needle is used to draw a sample of the fluid. The samples are typically taken from the hip bone. The samples go to a lab for testing.
- Tests to look for the Philadelphia chromosome. Specialized tests are used to analyze blood or bone marrow samples for the presence of the Philadelphia chromosome or the BCR-ABL gene. These tests may include fluorescence in situ hybridization analysis, also called FISH, and polymerase chain reaction test, also called PCR.
Phases of chronic myelogenous leukemia
The phase of chronic myelogenous leukemia refers to the aggressiveness of the disease. Your health care provider determines the phase by measuring the ratio of diseased cells to healthy cells in your blood or bone marrow. A higher ratio of diseased cells means chronic myelogenous leukemia is at a more advanced stage.
Phases of chronic myelogenous leukemia include:
- Chronic. The chronic phase is the earliest phase and generally has the best response to treatment.
- Accelerated. The accelerated phase is a transitional phase when the disease becomes more aggressive.
- Blast. The blast phase is a severe, aggressive phase that becomes life-threatening.
Treatment
The goal of chronic myelogenous leukemia treatment is to eliminate the blood cells that contain the BCR-ABL gene. For most people, treatment begins with targeted therapy that may help achieve a long-term remission of the disease.
Targeted therapy
Targeted therapy uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted therapy can cause cancer cells to die. In chronic myelogenous leukemia, the target of these medicines is the tyrosine kinase protein produced by the BCR-ABL gene. The medicines are called tyrosine kinase inhibitors, also known as TKIs.
TKIs are the initial treatment for people diagnosed with chronic myelogenous leukemia. Side effects of these targeted medicines include swelling or puffiness of the skin, nausea, muscle cramps, fatigue, diarrhea, and skin rashes.
Blood tests to detect the presence of the BCR-ABL gene are used to monitor the effectiveness of targeted therapy. If the disease doesn't respond or becomes resistant to targeted therapy, health care providers may consider other targeted therapy medicines or other treatments.
Health care providers haven't determined a safe point at which people with chronic myelogenous leukemia can stop taking targeted medicines. For this reason, most people continue to take targeted medicines even when blood tests show remission of the disease. In certain situations, you and your provider might consider stopping treatment with targeted medicines after discussing the benefits and risks.
Bone marrow transplant
A bone marrow transplant, also called a stem cell transplant, is the only treatment that can cure chronic myelogenous leukemia. However, it's usually reserved for people who haven't been helped by other treatments. That's because bone marrow transplants have risks and carry a high rate of serious complications.
During a bone marrow transplant, high doses of chemotherapy medicines are used to kill the blood-forming cells in your bone marrow. Then blood stem cells from a donor are infused into your bloodstream. The new cells form healthy blood cells to replace the diseased cells.
Chemotherapy
Chemotherapy uses strong medicines to kill cancer cells. Chemotherapy medicines are sometimes combined with targeted therapy to treat aggressive chronic myelogenous leukemia. Side effects of chemotherapy medicines depend on which medicines you take.
Clinical trials
Clinical trials are studies of new treatments. These studies provide a chance to try the latest treatments. The risk of side effects might not be known. Ask your health care provider if you might be able to be in a clinical trial.
Alternative medicine
No alternative medicines have been found to treat chronic myelogenous leukemia. But alternative medicine may help you cope with fatigue, which is common in people with chronic myelogenous leukemia.
You might experience fatigue as a symptom of your disease, a side effect of treatment or as part of the stress that comes with living with a chronic condition. Your health care provider can treat fatigue by controlling the underlying causes, but sometimes medicines alone aren't enough.
You may find relief through alternative therapies, such as:
- Exercise.
- Journal writing.
- Massage.
- Relaxation techniques.
- Yoga.
Talk to your provider about your options. Together you can devise a plan to help you cope with fatigue.
Lifestyle and home remedies
For many people, chronic myelogenous leukemia is a disease they will live with for years. Many will continue treatment with targeted therapy indefinitely. Some days, you may feel sick even if you don't look sick. And some days, you may just be sick of having cancer. Try these self-care measures to help you adjust and cope with a chronic illness:
- Talk to your health care provider about your side effects. Powerful cancer medicines can cause many side effects. Those side effects often can be managed with other medicines or treatments. You don't have to handle them without help.
- Don't stop treatment on your own. If you develop side effects, such as skin rashes or fatigue, don't quit your medicines without talking to your health care provider. Likewise, don't stop taking your medicines if you feel better and think your disease may be gone. If you stop taking medicines, your disease can quickly return, even if you've been in remission.
- Ask for help if you're having trouble coping. Having a chronic condition can be emotionally overwhelming. Tell your provider about your feelings. Ask for a referral to a counselor or another specialist with whom you can talk.
Coping and support
Facing a serious illness might make you feel worried. With time, you'll find ways to cope with your feelings, but you may find comfort in these strategies:
-
Learn enough about chronic myelogenous leukemia to make decisions about your care. The term "leukemia" can be confusing, because it refers to a group of cancers that affect the bone marrow and blood. Don't waste time gathering information that doesn't apply to your kind of leukemia.
Ask your health care team to write down information about your specific disease. Then narrow your search and seek out only trusted, reputable sources, such as the Leukemia & Lymphoma Society.
-
Stay connected to friends and family. Your cancer diagnosis can be stressful for friends and family, too. Try to keep them involved in your life.
Your friends and family will likely ask if there's anything they can do to help you. Think of tasks you might like help with, such as caring for your home if you have to stay in the hospital or just listening when you want to talk.
You may find comfort in the support of a caring group of your friends and family.
- Find someone to talk with. Find someone you can talk to who has experience helping people facing a life-threatening illness. Ask your provider to suggest a counselor or medical social worker you can talk with. For support groups, contact the American Cancer Society or ask your health care team about local groups.
Preparing for an appointment
Start by making an appointment with your primary care provider if you have any symptoms that worry you. If blood tests or other tests and procedures suggest leukemia, your provider may refer you to a specialist in the treatment of blood and bone marrow diseases and conditions, called a hematologist.
Because appointments can be brief, and because there's often a lot to discuss, it's a good idea to be prepared. Here's some information to help you get ready, and what to expect from your provider.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your health care provider.
Your time with your health care provider is limited, so prepare a list of questions to help make the most of your time together. List questions from most important to least important in case time runs out.
For chronic myelogenous leukemia, some basic questions to ask your provider include:
- Can you explain what my test results mean?
- Do you recommend any other tests or procedures?
- What is the phase of my CML?
- What are my treatment options?
- What side effects are likely with each treatment?
- How will treatment affect my daily life?
- Which treatment options do you think are best for me?
- How likely is it that I'll achieve remission with the treatments you recommend?
- How quickly must I make a decision on my treatment?
- Should I get a second opinion from a CML specialist? What will that cost, and will my insurance cover it?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared to ask, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
Your health care provider is likely to ask you a number of questions. Being ready to answer them may allow time later to cover other points you want to address. Your provider may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


