Overview
Benign peripheral nerve tumors are tumors that form on peripheral nerves. The peripheral nerves link the brain and spinal cord to other parts of the body. These nerves control muscles that allow you to walk, blink, swallow, pick things up and do other activities. Benign tumors are not cancerous.
Several different types of tumors may form on the peripheral nerves. While some are caused by genetics, the cause of these tumors is usually not known.
Although most of these types of tumors are not cancerous, they can cause nerve damage and loss of muscle control. It's important to see your healthcare professional if you have a lump or if you have pain, tingling, numbness or muscle weakness.
Types
Peripheral nerve tumors affect nerves by growing within them or by pressing against them. Peripheral nerve tumors that grow within nerves are called intraneural tumors. The tumors that press against nerves are called extraneural tumors. Most peripheral tumors are not cancer. These are known as benign tumors. Different types of benign peripheral nerve tumors include:
-
Schwannoma. A schwannoma is the most common benign peripheral nerve tumor in adults. These nerve sheath tumors are called schwannomas because they are made up of Schwann cells. Schwann cells surround the nerves.
These tumors usually grow slowly. If you develop a schwannoma in an arm or leg, you might notice a mass. But you might have a schwannoma for years before noticing it.
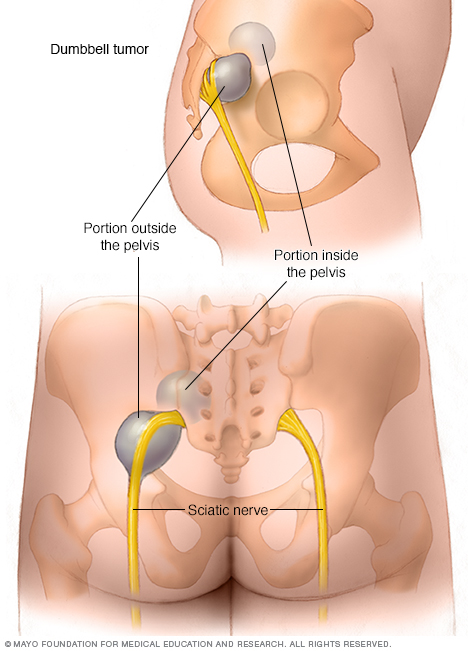
A schwannoma typically comes from a single bundle of nerve fibers, called a fascicle, within the main nerve. Some schwannomas grow and form irregular shapes within the spine or pelvis, such as dumbbell tumors. When a schwannoma grows, more fascicles are at risk when trying to remove the tumor safely.
Schwannomas most commonly occur alone. Occasionally some people have several of them in the arms, legs or body. This is a condition called schwannomatosis.
A rare schwannoma near the brainstem, known as an acoustic neuroma, can cause trouble with balance or hearing. This type of tumor also is known as a vestibular schwannoma. It sometimes occurs in people with a condition called NF2-related schwannomatosis. If acoustic neuromas aren't treated and they continue to grow, they can affect nearby nerves and press on the brainstem.
-
Neurofibroma. This common type of benign nerve tumor tends to form in the center of a nerve. A neurofibroma might arise from several nerve bundles and tends to cause mild symptoms. A neurofibroma most commonly develops in people who have a genetic condition that causes tumors to grow on nerves. This condition is known as neurofibromatosis type 1 (NF1).
Symptoms of NF1 include skin color changes and benign tumors on the skin. Some people who have NF1 develop other conditions. These conditions include bone changes, such as a curved spine, and an eye nerve tumor called an optic glioma. People with NF1 are at risk of developing a malignant peripheral nerve sheath tumor.
- Perineurioma. This rare benign peripheral nerve tumor arises from perineurial cells, a type of cell that surrounds the peripheral nerve sheath. A perineurioma can form within a nerve, called an intraneural perineurioma. It also may form in soft tissue next to a nerve, called an extraneural perineurioma. An intraneural perineurioma happens most often in children and young adults. It typically causes gradually progressive weakness in an arm or leg.
- Lipoma. Slow-growing fat cells cause this benign, soft lump that usually appears under the skin on the neck, shoulders, back or arms. A lipoma near a nerve can squeeze it. Usually, though, a lipoma causes no pain or other problems. Your healthcare professional might want to monitor a lipoma through regular checkups.
- Ganglion cyst. Some ganglion cysts come from an injury, but most have no known cause. They commonly form near joints, such as the wrist, and can cause pain and interfere with everyday activities. Some go away without treatment, but ganglion cysts that press on or are in nerves need to be treated.
Symptoms
Symptoms depend on the location of the benign peripheral nerve tumor and the nerves and tissues it affects. Symptoms may include:
- Swelling or a lump under your skin.
- Pain, tingling or numbness.
- Weakness or loss of function in the affected area.
- Dizziness or loss of balance.
A benign peripheral nerve tumor can cause symptoms if it presses on the nerve in which it is growing. It also can press on nearby nerves, blood vessels or tissues.
As a tumor grows, it may be more likely to cause symptoms. But even small tumors can cause symptoms.
Causes
The cause of benign peripheral nerve tumors usually isn't known. Some are passed down in families.
Risk factors
Risk factors may be different based on the type of benign peripheral nerve tumor.
For neurofibromas, having the genetic condition known as neurofibromatosis type 1 (NF1) is a risk factor. NF1 can cause someone to have several neurofibromas. But most people who have neurofibromas don't have NF1.
People with NF1 are also at increased risk for developing a malignant peripheral nerve sheath tumor. It’s important for them to check in often with a health care professional to monitor that risk.
For schwannomas, having the gene that causes schwannomatosis is a risk factor.
Diagnosis
To diagnose a peripheral nerve tumor, your healthcare professional runs tests to find where the tumor is located and what type of tumor it is.
Tests
You might need one or more of the following tests.
- MRI. This is the preferred method for imaging peripheral nerve tumors. This scan uses a magnetic field and radio waves to produce a detailed 3D view of the nerves and surrounding tissue. It can help determine whether you have a tumor and whether the tumor is inside or outside the nerve.
- CT scan. A CT scanner rotates around the body to record a series of images. This test is not as useful as an MRI in diagnosing a peripheral nerve tumor. However, your healthcare professional might recommend it if you can't have an MRI or if they need amore details about the bone near the tumor.
- Electromyogram (EMG). This test records the electrical activity in a muscle when you try to move it. It is used to help locate the tumor and identify which nerves are involved.
- Nerve conduction study. You're likely to have this test along with your EMG. It measures how quickly your nerves carry electrical signals to your muscles.
- Tumor biopsy. If imaging tests identify a nerve tumor, your healthcare professional might remove and study a small sample of cells from your tumor. This is known as a biopsy. Depending on the tumor's size and location, you might need local or general anesthesia during the biopsy. The biopsy might be done with a needle with the help of imaging, or it might be done during surgery.
- Nerve biopsy. To help diagnose the type of tumor, your healthcare professional may take a nerve biopsy. This involves taking a small sample of the tissue and sending it to a lab, where it's studied to look for signs of cancer.
Treatment
Treatment of peripheral nerve tumors involves either surgical removal or watching the tumor for changes. If there's a low chance that the tumor may become cancerous and if it isn't causing symptoms, you might not need surgery.
Your healthcare professional also might recommend observation if your tumor is in a place that makes it hard to remove. Observation includes regular checkups and imaging tests to see if the tumor is growing.
Surgery may be needed if there is a concern that the tumor is cancerous. The tumor also may be surgically removed if it is large or causing pain or other symptoms, such as weakness, numbness or tingling.
Preparing for an appointment
You might be referred to a doctor who specializes in nervous system conditions, known as a neurologist. Or you may be referred to a doctor trained in brain and nervous system surgery, known as a neurosurgeon.
Here's some information to help you get ready for your appointment, and to know what to expect.
What you can do
- Write down when you first noticed symptoms and whether they have changed with time.
- Write down your key medical information, including any surgeries.
- Make a list of all your medications, vitamins or supplements, including the doses.
- Find out if anyone in your family has ever had similar problems.
- Ask a family member or friend to accompany you, to help you remember what you learn during the appointment.
- Write down questions to ask during the appointment.
Questions to ask your doctor
- What's the most likely cause of the problem?
- What kinds of tests do I need?
- What treatments are available?
- I have other health conditions. How can I best manage them together?
In addition to asking questions you've prepared, don't hesitate to ask other questions that come up during your appointment.
What to expect from your doctor
Your healthcare professional asks a number of questions. Being ready to answer them may make time to go over points you want to discuss in-depth. You might be asked:
- Do you have pain? Where is it?
- Do you have any weakness, numbness or tingling?
- Have your symptoms been continuous or occasional?
- What treatments have you tried already for these problems?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


