Overview
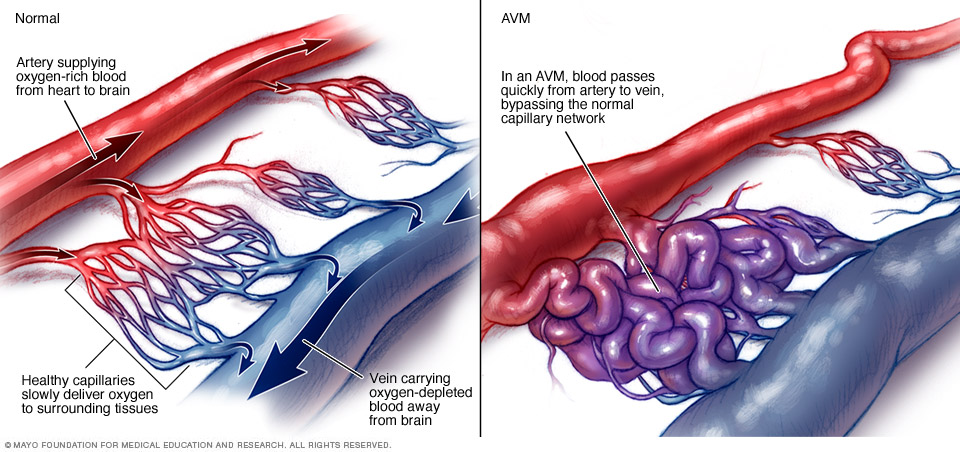
An arteriovenous malformation, also known as an AVM, is a tangle of blood vessels that creates irregular connections between arteries and veins. This disrupts blood flow and prevents tissues from receiving oxygen. An AVM can occur anywhere in the body, including in the brain.
Arteries move oxygen-rich blood from the heart to the brain and other organs. Veins drain the oxygen-depleted blood back to the lungs and heart. When an AVM disrupts this critical process, surrounding tissues might not get enough oxygen.
Because the tangled blood vessels in an AVM do not form properly, they can weaken and burst. If an AVM in the brain bursts, it can cause bleeding in the brain, which can lead to a stroke or brain damage. Bleeding in the brain is known as a hemorrhage.
Read more about brain AVM (arteriovenous malformation).
The cause of AVMs is not clear. Rarely, they are passed down in families.
Once diagnosed, a brain AVM often can be treated to prevent or reduce the risk of complications.
Symptoms
Symptoms of an arteriovenous malformation, also known as an AVM, can vary. Sometimes an AVM doesn't cause symptoms. The AVM can be found while getting images for another health concern.
Often the first symptoms appear after bleeding occurs. Besides bleeding, symptoms can include:
- Trouble with thinking that gets worse over time.
- Headaches.
- Nausea and vomiting.
- Seizures.
- Loss of consciousness.
Other possible symptoms include:
- Weak muscles, such as weakness in the legs.
- Loss of movement and feeling in one part of the body, known as paralysis.
- Loss of coordination that can cause trouble with walking.
- Trouble doing tasks that require planning.
- Back pain.
- Dizziness.
- Vision problems. This may include losing part of the field of vision, trouble moving the eyes or swelling of part of the optic nerve.
- Trouble with speech or understanding language.
- Numbness, tingling or sudden pain.
- Memory loss or dementia.
- Seeing or hearing things that aren't there, known as hallucinations.
- Confusion.
Children and teens might have trouble with learning or behavior.
One type of AVM called a vein of Galen malformation causes symptoms that appear at or shortly after birth. A vein of Galen malformation occurs deep inside the brain. Signs can include:
- A buildup of fluid in the brain that causes the head to be larger than usual.
- Swollen veins on the scalp.
- Seizures.
- Failure to thrive.
- Congestive heart failure.
When to see a doctor
Seek medical attention if you have any of the symptoms of an AVM, such as headaches, dizziness, vision problems, seizures and changes in thinking. Many AVMs are found during testing for a different condition, such as during a CT scan or an MRI.
Causes
An arteriovenous malformation happens when arteries and veins connect in an irregular way. Experts don't understand why this happens. Certain genetic changes might play a role, but most types are not usually passed down in families.
Risk factors
Rarely, having a family history of an arteriovenous malformation can increase your risk. But most types aren't inherited.
Certain hereditary conditions can increase your risk of an arteriovenous malformation. These include hereditary hemorrhagic telangiectasia, also known as Osler-Weber-Rendu syndrome.
Complications
The most common complications of an arteriovenous malformation are bleeding and seizures. Bleeding can cause brain damage and may cause death if you don't get treated.
Diagnosis
To diagnose an arteriovenous malformation, also known as an AVM, your healthcare professional reviews your symptoms and gives you a physical exam.
Your healthcare professional may listen for a sound called a bruit. A bruit is a whooshing sound caused by blood quickly flowing through arteries and veins of an AVM. It sounds like water rushing through a narrow pipe. A bruit can interfere with your hearing or sleep or cause emotional distress.
Tests commonly used to help diagnose AVM include:
- Cerebral angiography. This test looks for an AVM in the brain. Also called arteriography, this test uses a special dye called a contrast agent injected into an artery. The dye highlights the blood vessels to better show them on X-rays.
- CT scan. These scans can help show bleeding. CT scans use X-rays to create images of the head, brain or spinal cord.
- CT angiography. This test combines a CT scan with an injection of a dye to help find an AVM that is bleeding.
- MRI. An MRI uses powerful magnets and radio waves to show detailed images of tissues. An MRI can pick up on small changes in these tissues.
- Magnetic resonance angiography, also known as an MRA. MRA captures the pattern and the speed and distance of blood flow through the irregular vessels.
- Transcranial doppler ultrasound. This test can help diagnose an AVM and tell whether the AVM is bleeding. The test uses high-frequency sound waves aimed at arteries to create an image of blood flow and its speed.
Treatment
Treatment of an arteriovenous malformation, also known as an AVM, depends on where it is found, your symptoms and the risks of treatment. Sometimes an AVM is monitored with regular imaging tests to watch for changes. Other AVMs require treatment. Your healthcare professional may recommend conservative management if the AVM hasn't burst and you are not at high risk of the AVM bleeding.
When deciding whether to treat an arteriovenous malformation, healthcare professionals consider:
- Whether the AVM has bled.
- Whether the AVM is causing symptoms other than bleeding.
- Whether the AVM is in a part of the brain where it can safely be treated.
- Other characteristics of the AVM, such as its size.
Medicines
Medicines can help manage symptoms related to an arteriovenous malformation, such as seizures, headaches and back pain.
Surgery
The main treatment of an AVM is surgery. Surgery might completely remove the arteriovenous malformation. This treatment might be recommended if there is a high risk of bleeding. Surgery usually is an option if the AVM is in an area where removing it has little risk of causing damage to brain tissue.
Endovascular embolization is a type of surgery that involves threading a catheter through the arteries to the arteriovenous malformation. Then a substance is injected to close parts of the AVM to reduce the blood flow. This might be done before brain surgery or radiosurgery to help reduce the risk of complications.
Sometimes stereotactic radiosurgery is used to treat an AVM. The treatment uses intense, highly focused beams of radiation to damage the blood vessels. This helps stop the blood supply to the AVM.
You and your healthcare team discuss whether to treat your AVM, weighing the possible benefits against the risks.
Follow-up
After treatment for an arteriovenous malformation, you might need regular follow-up visits with your healthcare team. You also might need more imaging tests to make sure that the AVM has been successfully treated and that the malformation has not come back. You'll also need regular imaging tests and follow-up visits with your healthcare team if your AVM is being monitored.
Coping and support
Learning that you have an arteriovenous malformation can be concerning. But you can take steps to cope with the emotions that may come with your diagnosis and recovery, such as:
- Learn about arteriovenous malformations, also known as AVMs. This can help you make informed decisions about your care. Ask about the size and location of the AVM, and what that means for your treatment options.
- Accept your emotions. Complications of AVM, such as hemorrhage and stroke, can affect you emotionally.
- Keep friends and family close. Friends and family can provide the practical support you may need. Ask the people you're close to if they can come to healthcare appointments with you. Lean on your friends and family for emotional support.
- Talk about how you feel. Talking to a friend, family member, counselor, social worker or clergy member may help. You also might find comfort in a support group. Ask your healthcare team about support groups in your area. Or reach out to a national organization, such as the American Stroke Association or The Aneurysm and AVM Foundation.
Preparing for an appointment
An arteriovenous malformation, also known as an AVM, might be diagnosed in an emergency situation. Some AVMs are diagnosed right after bleeding, known as a hemorrhage, or a seizure. An AVM also may be found after other symptoms prompt imaging scans.
But sometimes an AVM is found during testing for another condition. You might then be referred to a doctor trained in brain and nervous system conditions, such as a neurologist, interventional neuroradiologist or neurosurgeon.
Here are some things you can do to get ready for your appointment.
What you can do
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance.
- Write down your symptoms, including any that may not seem related to the reason for which you scheduled the appointment.
- Make a list of all medicines, vitamins and supplements you're taking, including doses.
- Ask a family member or friend to come with you, if possible. Someone else might help you remember the information you're given.
- Write down questions to ask. Don't be afraid to ask questions that may come up during your appointment.
For AVM, some basic questions to ask include:
- What are other possible causes for my symptoms?
- What tests are needed to confirm the diagnosis?
- What are my treatment options and the pros and cons for each?
- What results can I expect?
- What kind of follow-up should I expect?
What to expect from your doctor
Your neurologist is likely to ask about your symptoms, if any. Your neurologist also may do a physical exam and schedule tests to confirm the diagnosis.
The tests gather information about the size and location of the AVM to help direct your treatment options. You may be asked:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


