Overview
Alcoholic hepatitis is swelling, called inflammation, of the liver caused by drinking alcohol. Drinking alcohol destroys liver cells.
Alcoholic hepatitis most often happens in people who drink heavily over many years. But the link between drinking and alcoholic hepatitis isn't simple. Not all heavy drinkers get alcoholic hepatitis. And some people who drink much less get the disease.
If you're diagnosed with alcoholic hepatitis, you must stop drinking alcohol. People who keep drinking alcohol have a high risk of serious liver damage and death.

Symptoms
The most common sign of alcoholic hepatitis is yellowing of the skin and whites of the eyes, called jaundice. The yellowing of the skin might be harder to see on Black and brown people.
Other symptoms include:
- Loss of appetite.
- Nausea and vomiting.
- Belly tenderness.
- Fever, often low grade.
- Tiredness and weakness.
People with alcoholic hepatitis tend to be malnourished. Drinking large amounts of alcohol keeps people from being hungry. And heavy drinkers get most of their calories from alcohol.
Other symptoms that happen with severe alcoholic hepatitis include:
- Fluid buildup in the belly, called ascites.
- Being confused and acting oddly due to a buildup of toxins. The healthy liver breaks these toxins down and gets rid of them.
- Kidney and liver failure.
When to see a doctor
Alcoholic hepatitis is a serious, often deadly disease.
See a healthcare professional if you:
- Have symptoms of alcoholic hepatitis.
- Can't control your drinking.
- Want help cutting back on your drinking.
Causes
Alcoholic hepatitis is caused by damage to the liver from drinking alcohol. Just how alcohol damages the liver and why it does so only in some heavy drinkers isn't clear.
These factors are known to play a role in alcoholic hepatitis:
- The body's way of breaking down alcohol makes highly toxic chemicals.
- These chemicals trigger swelling, called inflammation, that destroys liver cells.
- Over time, scars replace healthy liver tissue. This keeps the liver from working well.
- This scarring, called cirrhosis, can't be fixed. It's the final stage of alcoholic liver disease.
Other factors that can be involved with alcoholic hepatitis include:
- Other types of liver disease. Alcoholic hepatitis can make chronic liver diseases worse. For instance, if you have hepatitis C and drink, even a little, you're more likely to get liver scarring than if you don't drink.
- Lack of nutrition. Many people who drink heavily don't get enough nutrients because they eat poorly. And alcohol keeps the body from using nutrients as it should. Lack of nutrients can damage liver cells.
Risk factors
The major risk factor for alcoholic hepatitis is the how much alcohol you drink. It isn't known how much alcohol it takes to cause alcoholic hepatitis.
Most people with this condition have had at least seven drinks a day for 20 years or more. This can mean 7 glasses of wine, 7 beers, or 7 shots of spirits.
However, alcoholic hepatitis can happen to people who drink less and have other risk factors, including:
- Sex. Women seem to have a higher risk of getting alcoholic hepatitis. That might be because of how alcohol breaks down in women's bodies.
- Obesity. Heavy drinkers who are overweight might be more likely to get alcoholic hepatitis. And they might be more likely to go on to get liver scarring.
- Genes. Studies suggest that genes might be involved in alcohol-induced liver disease.
- Race and ethnicity. Black and Hispanic people might be at higher risk of alcoholic hepatitis.
- Binge drinking. Having five or more drinks in about two hours for men and four or more for women might increase the risk of alcoholic hepatitis.
Complications
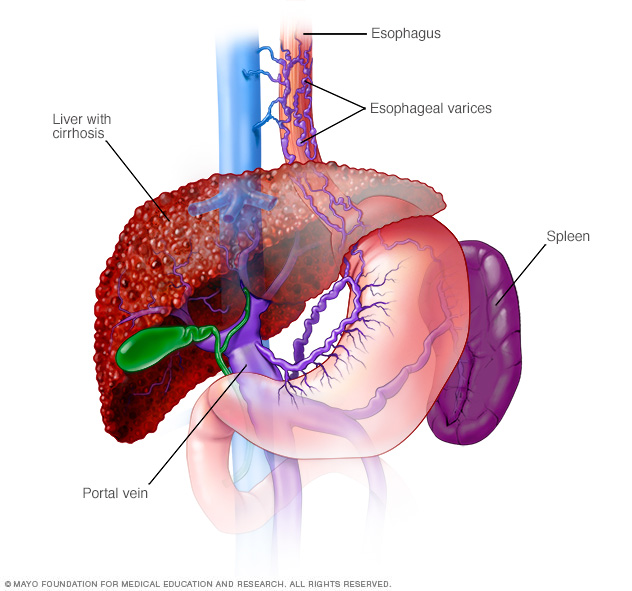
Complications of alcoholic hepatitis are caused by scar tissue on the liver. Scar tissue can slow blood flow through the liver. That can raise pressure in a major blood vessel called the portal vein and cause a buildup of toxins.
Complications include:
-
Enlarged veins, called varices. Blood that can't flow freely through the portal vein can back up into other blood vessels in the stomach and the tube through which food passes from the throat to the stomach, called the esophagus.
These blood vessels have thin walls. They're likely to bleed if filled with too much blood. Heavy bleeding in the upper stomach or esophagus is life-threatening and needs medical care right away.
- Ascites (ah-SITE-ees). Fluid that builds up in the belly might get infected and need treatment with antibiotics. Ascites isn't life-threatening. But it most often means advanced alcoholic hepatitis or cirrhosis.
- Confusion, drowsiness and slurred speech, called hepatic encephalopathy. A damaged liver has trouble removing toxins from the body. The buildup of toxins can damage the brain. Severe hepatic encephalopathy can cause a coma.
- Kidney failure. A damaged liver can affect blood flow to the kidneys. This can damage the kidneys.
- Cirrhosis. This scarring of the liver can lead to liver failure.
Prevention
You might reduce your risk of alcoholic hepatitis if you:
- Drink alcohol in moderation, if at all. For healthy adults, moderate drinking means up to one drink a day for women and up to two drinks a day for men. The only certain way to prevent alcoholic hepatitis is to avoid all alcohol.
- Protect yourself from hepatitis C. Hepatitis C is a liver disease caused by a virus. Without treatment, it can lead to cirrhosis. If you have hepatitis C and drink alcohol, you're far more likely to get cirrhosis than if you don't drink.
-
Check before mixing medicines and alcohol. Ask your healthcare professional if it's safe to drink alcohol when taking your prescribed medicines. Read the warning labels on medicines you can get without a prescription.
Don't drink alcohol when taking medicines that warn against drinking alcohol while taking them. This includes pain relievers such as acetaminophen (Tylenol, others).
Diagnosis
Your healthcare professional does a physical exam and asks about your alcohol use, now and in the past. Be honest about your drinking. Your care professional might ask to talk to family members about your drinking.
Diagnosing liver disease might involve these tests:
- Liver function tests.
- Blood tests.
- An ultrasound, CT or MRI scan of the liver.
- A liver biopsy, if other tests and imaging don't give a clear diagnosis or if you are at risk of other causes of hepatitis.

Treatment
Treatment for alcoholic hepatitis involves quitting drinking as well as therapies to ease the symptoms of liver damage.
Quitting drinking
If you've been diagnosed with alcoholic hepatitis, you need to stop drinking alcohol and never drink alcohol again. It's the only way that might reverse liver damage or keep the disease from getting worse. People who don't stop drinking are likely to have some life-threatening health problems.
If you depend on alcohol and want to stop drinking, your healthcare professional can suggest a therapy that meets your needs. It can be harmful to stop drinking all at once. So discuss a plan with your healthcare professional.
Treatment might include:
- Medicines.
- Counseling.
- Alcoholics Anonymous or other support groups.
- Outpatient or live-in treatment program.
Treatment for malnutrition
Your healthcare professional might suggest a special diet to fix poor nutrition. You might be referred to an expert in diet to manage disease, called a dietitian. A dietitian can suggest ways to eat better to make up for the vitamins and nutrients you lack.
If you have trouble eating, your care professional might suggest a feeding tube. A tube is passed down the throat or through the side and into the stomach. A special nutrient-rich liquid diet is then passed through the tube.
Medicines to reduce liver swelling, called inflammation
These might help severe alcoholic hepatitis:
- Corticosteroids. These medicines might help some people with severe alcoholic hepatitis live longer. However, corticosteroids have serious side effects. They're not likely to be used if you have failing kidneys, stomach bleeding or an infection.
- Pentoxifylline. Your healthcare professional might suggest this medicine f you can't take corticosteroids. How well pentoxifylline works for alcoholic hepatitis isn't clear. Study results differ.
- Other treatment. N-acetylcysteine may help some people with alcoholic hepatitis. More study is needed.
Liver transplant
For many people with severe alcoholic hepatitis, the risk of dying is high without a liver transplant.
In the past, those with alcoholic hepatitis have not been given new livers. This is because of the risk that they'll continue drinking after transplant. But recent studies suggest that well-chosen people with severe alcoholic hepatitis have survival rates after a transplant similar to people with other types of liver disease who get liver transplants.
For transplant to be an option, you would need:
- To find a program that works with people who have alcoholic hepatitis.
- To follow the rules of the program. This includes making a promise not to drink alcohol for the rest of your life.
Preparing for an appointment
You might be referred to a digestive disease specialist, called a gastroenterologist.
What you can do
When you make the appointment, ask if there's anything you need to do before certain tests, such as not eating or drinking.
Make a list of:
- Your symptoms, including any that don't seem linked to the reason you made the appointment, and when they began.
- All medicines, vitamins and supplements you take, including doses.
- Key medical information, including other conditions you have.
- Key personal information, including recent changes or stressors in your life. Keep track of how much alcohol you drink for a few days for your healthcare professional.
- Questions to ask your healthcare professional.
Have a relative or friend go with you, if possible, to help you remember the information you're given.
Questions to ask your doctor
- What's the most likely cause of my symptoms? Are there other possible causes?
- Do I have any other liver disease?
- Is there scarring of my liver?
- What tests do I need? How do I prepare for them?
- Is my condition likely to go away or be long-lasting?
- What treatment do you suggest?
- I have other health problems. How can I best manage these conditions together?
Be sure to ask all the questions you have about your condition.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, including:
- How bad are your symptoms? Do they come and go, or do you have them all the time?
- Does anything improve your symptoms or make them worse?
- Have you had hepatitis or yellowing of the skin or whites of your eyes?
- Do you use illicit drugs?
- Have you ever felt you should cut down on drinking or felt guilty or bad about your drinking?
- Are your family members or friends worried about your drinking? Have you been arrested or had other problems because of your drinking?
- Do you get angry or upset when anyone talks about your drinking?
- Do you feel guilty about drinking?
- Do you drink in the morning?
© 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


